|
| |
Issue no. 47 - December 1991
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 47 - December
1991
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  Page 1 2
Page 1 2
Ask, listen... but don't forget to look
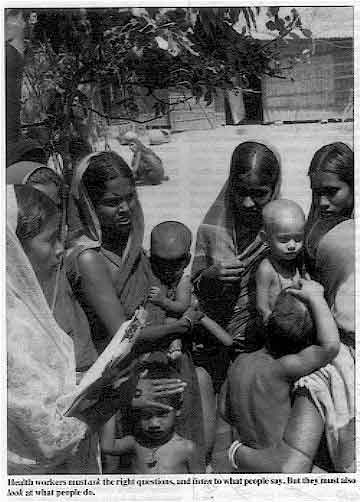 |
Health workers must ask the right
questions, and listen to what people say. But they must also look
at what people do. Helping families to make their homes safer is an important part of the prevention and
control of diarrhoea1ldisease. This issue of DD looks at questions
which relate to hygiene behaviour: how people handle food, water and wastes - human and
animal excreta, and garbage of all kinds. Faecal-oral transmission of diarrhoea germs is
the polite way to describe tiny amounts of shit somehow getting into human mouths. This
danger has to be reduced. Better sanitation and cleaner water supply can help but. to make
a real difference. families also need access to appropriate hygiene education.
|
Real understanding To be effective, this education must be based on genuine understanding of how people
think about hygiene in their daily lives and why they do as they do. Suggested changes
must fit the local environment, which should include religious and cultural traditions as
well as household and economic circumstances. Aspects of looking at hygiene behaviour are
discussed on pages 2, 3 and 4. and pages 5 and 6 show how some particularly difficult
environmental conditions are linked with persistent diarrhoea due to worms. See what people do Ansvvers to questions from readers about ORT on="#page7">page 7 also show
the importance of understanding what people do and why. This means asking questions and
listening to what people say. But, because the asking of a question can influence the
answer, it is equally vital always to look at what people actually do. We have to have the
whole picture if we hope to improve behaviour.
|
In this issue:
- Finding out about hygiene behaviour
- Worms and child health
- Problems with ORT? Your questions answered
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  1 Page 2 3 1 Page 2 3
| Diarrhoea and hygiene behaviour |
Learning about what people do and why
DD explains why it is important to understand hygiene behaviour and
how this knowledge can help to reduce the spread of diarrhoeal infections. How people carry out day-to-day personal and domestic activities that relate to the
transmission of infections, including diarrhoea, is called 'hygiene behaviour'. Hygiene
behaviour is important because it affects the household level of contamination by germs,
and the extent to which those germs can infect the family. Diarrhoea-causing germs are
most commonly spread from person to person by the faecal-oral route. Hygiene behaviours
that influence diarrhoea transmission by this route include:
- where people defecate;
- whether and how hands are washed (or otherwise cleaned) after defecating. and before
preparing and eating food;
- how babies' faeces are disposed of;
- how water is stored and used; and
- how food is prepared and stored.
Why do we need to know about hygiene behaviour? People are likely to have fewer diarrhoea infections if they have access to clean
drinking water and good sanitation facilities. But, if hygiene behaviour is poor, the
health benefits resulting from provision of improved sanitation and water supplies will be
limited. Clean drinking water and better sanitation typically reduce diarrhoea incidence
by only 25 per cent (1). Interrupting faecal-oral transmission of germs
also depends on improving personal and domestic hygiene behaviours. Diarrhoeal disease control programmes have tried to improve hygiene behaviour by
introducing different interventions such as educating families about the importance of
domestic hygiene. Promoting improved hygiene has been shown to halve the number of
diarrhoea infections. But if these interventions fail, it is often because they have not
been appropriately designed or put into practice. This can be due to lack of understanding
about what people think about hygiene and why they behave in a particular way. Sometimes
it is also because the interventions have not been aimed at the behaviours which are most
responsible for spreading infections. It is therefore important to understand people's existing hygiene behaviour, and the
factors that determine it, so that health education interventions to change behaviour are
appropriate, and so that behaviour does change, leading to improvements in health.
Programmes also need to be aware that although people may know about the safest
practices, certain constraints may prevent them from actually doing things the
safest way. In Zimbabwe, Pauline Gwatirisa investigated why providing water and
sanitation had failed to reduce diarrhoeal and worm infections in poor rural communities.
Studying behaviour showed that, even when latrines were provided, defecation practices did
not always change. It was found that, although people agreed that their household toilet
was the safest place for excreta disposal, where their food gardens were several
kilometres distant from their homes, people pointed out that they would waste much time
and energy walking back home to use the toilet. They were therefore encouraged to bury
their faeces, or dig a small pit for faeces disposal near the gardens.
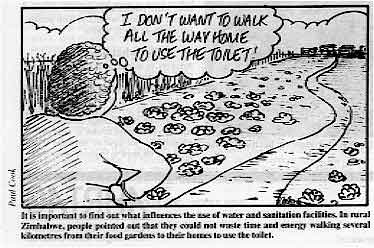 |
It is important to find out what influences the use of
water and sanitation facilities. In rural Zimbabwe, people pointed out that they could not
waste time and energy walking several kilometres from their food gardens to their homes to
use the toilet.
|
Most people in a community will have similar ways of doing things, but there will be
variations between families or individuals. Some ways of doing things are more likely to
increase infection spread than others, and may therefore be related to a higher rate of
diarrhoea infections. Studies help to find out which ways of behaving are most likely to
be linked to high rates of diarrhoea. Hygiene behaviour studies carried out before introducing
interventions can reveal:
- what people think and do about hygiene, and why they act in a particular way;
- the practices responsible for transmitting infection which the programme or intervention
should aim to change;
- which factors influence or limit the extent to which behaviour can be changed (such as
beliefs about cleanliness).
Similar studies after an intervention has been introduced also provide useful
information which helps to:
- monitor how well hygiene behaviour interventions are working;
- examine how water and sanitation programmes affect health and hygiene behaviour;
- identify the reasons why a programme might not be having an impact on the incidence of
diarrhoea.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  2 Page 3 4 2 Page 3 4
| Diarrhoea and hygiene behaviour |
How is hygiene behaviour studied? Hygiene behaviour studies should collect information from a large number of families if
the results are to be useful for programme planners. This is because it is important to
know that a significant proportion of people in the community behave in a particular way,
in order to design an appropriate intervention for the whole community, or to find out if
an intervention has been effective.
|
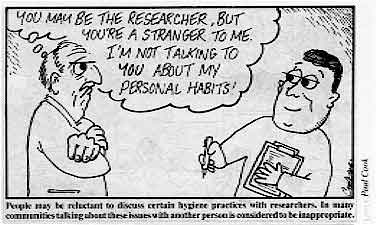
People may be reluctant to discuss certain hygiene practices
with researchers. In many communities talking about these issues with another person is
considered to be inappropriate.
Finding out what large numbers of people believe and do, and why they do it, is not
easy. Investigating how this information relates to disease is even harder. Behaviour is
much more difficult to study than whether water supplies are available. Behaviour is
difficult to define, often very variable and determined by cultural context. Identifying
'poor' behaviour can mean that people themselves are blamed for their ill
health.
|
 |
Researchers have developed various methods and practical techniques for collecting
information and to help them to identify and measure the behaviours that influence the
spread of infections, including diarrhoea. The field workers who carry out the study in
the community need training in how to use the techniques. It is helpful to start by
finding out more about the social and cultural background of the community, for example
family income and level of maternal education. Preliminary studies Preliminary studies, usually on a small scale, provide information for designing a
larger study. Such preliminary studies can ensure that a questionnaire uses the right
words to refer to behaviours common in the community. One technique used in these studies
is the focus group discussion, where, for example, small groups of women are encouraged to
discuss what they think and do about child health and hygiene practices, and give reasons
for why they do certain things.
|
Designing health education messages This study shows how information about hygiene behaviour was used to design effective
educational messages. Researchers in Bangladesh wanted to develop health education
messages to improve hygiene behaviour and reduce diarrhoea infections in children living
in poor areas of the capital city, Dhaka. Through comparing hygiene behaviour in two
different groups of families, the study identified which hygiene related practices were
most likely to be associated with high rates of diarrhoea infection. Using this
information the researchers designed appropriate health education messages aimed at
improving these practices. Diarrhoea incidence in children was recorded by asking mothers to mark episodes of
diarrhoea on special calendars designed for non-literate adults. Two groups of about 50
families with children under five were selected: one consisted of households in which the
children had the highest number of diarrhoea infections, and the other of those in which
incidence was lowest. Hygiene behaviour in both groups was studied to find out if there were things which
people did differently in each group and which might increase infection spread. In the
households in which there was a higher incidence of diarrhoea infections, the researchers
observed that:
- more mothers did not wash their hands before preparing food;
- infants were more likely to defecate in the family living area, and their faeces were
more likely to be found in this area;
- families were more likely to leave household waste uncovered in the living area, and
children were observed to put garbage in their mouths more often.
Simple health education messages focusing on these three behaviours were designed to
emphasise the need to:
- wash hands before food preparation:
- encourage children to defecate away from the house at a special site, or in a latrine;
- dispose of garbage and infant faeces safely.
A later study showed that these interventions succeeded in changing the three
behaviours and in reducing the number of diarrhoea episodes, particularly among two and
three year olds.
Clemens J D and Stanton B. 1987. An educational intervention for altering water-
sanitation behaviours to reduce childhood diarrhoea in urban Bangladesh. Am. J.
Epid. vol. 125: 284-301.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  3 Page 4 5 3 Page 4 5
| Diarrhoea and hygiene behaviour |
Interviews, questionnaires and surveys Surveys are a useful way to find out what water and sanitation facilities are available
for domestic use. These methods can also be used to explore accepted norms of behaviour,
that is, what most people think they should be doing. People may say they do one
thing, but actually behave differently. They will also only answer the questions they are
asked, so questions have to be well chosen, using information from preliminary studies. Vijay Kochar describes what happened during his research in West Bengal, in India: 'Wewere studying hookworm transmission in a village with no sanitation facilities. When
interviewed, villagers confirmed our expectations, saying that people have special places
for open air defecation, which are used only for that purpose. However, when I examined
the actual stool distribution around the village, I found it to be much more varied than
had been indicated in interviews, and saw that people use the defecation grounds for other
activities too, such as collecting wood.' Cultural factors can be a major obstacle to obtaining information. In Zimbabwe, researchers
found that it was difficult to collect data on the usage of sanitary facilities by older
people - in many communities it is not culturally appropriate to discuss such issues with
another person. It is not always necessary to question people about what they actually do. Sometimes
discovering what they think about hygiene can be useful in itself. One example of this is
a study in Papua New Guinea which was designed to find out what mothers believed
about the role of babies' faeces in spreading infection. not how they actually disposed of
infant faeces (2). Field workers completed a questionnaire during open discussions with mothers. The
information was then compared with the number of diarrhoea infections in their children
over a year. Children whose mothers believed that infant faeces were not a source of
infection were more likely to have had diarrhoea. This finding helped planners to design
an appropriate educational intervention for women about the infectiousness of babies'
faeces, and the need to dispose of them safely. Direct observation Direct observation enables researchers to compare people's hygiene behaviour in their
own homes with what they say they do. Seeing what people actually do, for example, about
storing and using water, can reveal hygiene practices that could increase the spread of
infection. In a study on water use in Bangladesh, in an area where most families had access
to clean water from handpumps, people were asked where they obtained their drinking water
(3). Although most said that they drank only handpump water, close
observation revealed that some people used contaminated pond water for many other
household purposes such as cleaning feeding bottles, and that the two sorts of water were
usually stored side by side in the home. This increased the risk of transmission of
infection from contaminated water. Direct observation is, however, a labour intensive method. In addition, people may
change their normal way of doing things when a researcher - usually a stranger to the
family - is present. Jane Baltazar comments on carrying out such a study in a poor community in Metro Manila
in the Philippines: 'We designed an "observation checklist". which
included sections for the observers to record practices related to young child defecation,
and maternal water handling and food preparation behaviour. However. we encountered a
major problem.
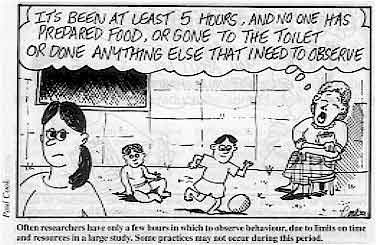 |
Often researchers have only a few hours in which to observe
behaviour, due to limits on time and resources in a large study. Some practices may not
occur during this period. Due to limits on time and resources. we could only spend one hour in each household.
|
Often the events we wanted to observe, like infant defecation or rubbish disposal, did
not occur during this time. Even when the interview was extended to five hours, these
behaviours were recorded in only 10 per cent of the households. Indirect observation Sometimes researchers do not have to observe how something is done. Instead they look
for and see signs that indicate that a person has done something in a certain way. For
example, a clean yard can mean that infant faeces have been swept up and disposed of
safely. These signs can be useful measures of behaviour and are easily observable even
during short interviews. Special arrangements should not be made for visits, since if
people are expecting a researcher to come to their homes they may change how they normally
do something. Conclusion The International Reference Centre for Community Water Supply and Sanitation (in The
Netherlands) is using the experience of a number of hygiene behaviour studies to draw up
guidelines to help programme planners to design cost effective and useful studies,
particularly in relation to water and sanitation programmes. These studies will enable
planners to introduce and monitor hygiene behaviour interventions that will best reduce
transmission of infection in their community. The guidelines will be published by the International Development Research Center in
1992. (Details will be included in a future issue of DD). DD would like to thank the following for permission to use papers presented
at the Workshop on Measurement of Hy giene Behaviour, held in Oxford, UK, in April 1991:
Dr Sandy Cairncross, Dr Jane Baltazar, Dr Pauline Gwatirisa, Dr Patricia Haggarty and
Professor Vijay Kochar. 1. Esrey S et al, 1985. Interventions for the control of diarrhoeal
diseases among young children: improving water supplies and excreta disposal
facilities. WHO Bulletin. vol 63:757-772.
2. Bukenya et al, 1990 The relationship of mothers' perception of
babies' faeces and other factors to childhood diarrhoea in an urban settlement of Papua
New Guinea. Ann. Trop. Paed. vol 10: 185-189
3. Zeitlyn S and Islam F, 1991. The use of soap and water in
two Bangladeshi cornmrnities: implications for the transmission of diarrhoea.
(Forthcomintg publication)
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  4 Page 5 6 4 Page 5 6
Water and sanitation are not enough
Chris Smith discusses why worms, often associated with
diarrhoea, are still a major problem for young children in Palestinian refugee camps,
despite widespread access to piped water and sanitation facilities. The Gaza Strip has a population of approximately 700,000 Palestinians living on a
narrow strip of land about 25 miles long and 5 miles wide. The area is part of the
Occupied Territories, and lies on the east coast of the Mediterranean Sea, bordering Egypt
to the south and Israel to the east. Most people are refugees, with over half living in
seven camps administered by the United Nations Relief and Works Agency. The vast majority of people living in the refugee camps have access to both a piped
water supply with a tap in their house or yard (98 per cent) and some kind of latrine (97
per cent). However, infestations by roundworm (Ascaris lumbricoides) and whipworm (Trichuris
trichuria) are endemic (the latter having a known association with persistent
diarrhoea). In 1988 a study was carried out to try to find out why these infestations are
so common in spite of high levels of access to water and sanitation. To start with, stool samples were collected from young children coming to the clinics
in the camps. Tests on the samples showed that in all the camps up to half the children
treated had worm infestations. Following this initial sampling, a community based survey
was carried out in one of the camps (Beach Camp), in which infection levels were measured
in children aged under 10 years. Of 137 children tested, 10 per cent had roundworm and 26
per cent had whipworm, showing a typical age prevalence pattern (see table).
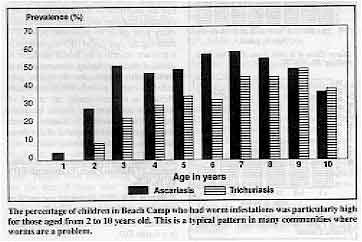 |
The percentage of children in Beach Camp who had worm
infestations was particuiarly high for those aged from 2 to 10 years old. This is a
typical pattern in many communities where worms are a problem. |
Seventy-four sand samples from the camp were analysed for the presence of helminth ova
(eggs), 23 from sandy courtyards and 51 from the street; 61 per cent of the yard samples
and 75 per cent of the street samples contained Ascaris lurnbricoides ova,
although none contained Trichuris trichuria.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  5 Page 6 7 5 Page 6 7
Continued from previous page Investigating the problem
Environmental conditions and hygiene behaviour were analysed to find out why so many
children still had worm infestations: household questionnaires included sections on house
and street environments, hygiene related knouledge and attitudes, and hygiene practices of
children. Some households were selected for observation of hygiene related behaviour. The
results suggested that the persistence of worm infections was due to a combination of:
- Inadequate sanitation
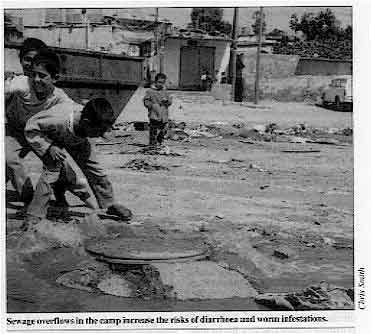
Almost every house in the camp had a latrine, in some areas
connected to a pit. While some pits were linked to a newly installed underground piped
sewerage system, others overflowed into the street.These pit overflows provided a regular source of pollution and a suitable damp
environment for helminth ova to survive (until they contaminated food, water or people's
hands and were swallowed).
|
Sewage overflows in the camp increase the risks of diarrhoea and worm
infestations.
- Seasonal flooding
In winter during heavy rains, local flooding washed the faecal contents from latrine pits
to the street surface. Piped sewers flooded the streets during these rainstorms, spreading
faecal materials throughout the camp.
|
 |
- Poor disposal of faeces
During observation, researchers saw that the faeces of young children were being deposited
in household yards, either through direct defecation or through leakage from nappies.
Traces of human faeces were observed in 10 per cent of the houses during the survey.
Faecal remains were eventually swept or washed away - usually into the street.
Prevention and treatment The overflow problem can be solved by the installation of piped sewerage networks in
the camps, while health education can help to improve hygiene practices. But the problem
of winter flooding will be more difficult to solve in the near future. Without a storm
drainage system, the sewers will continue to flood the street surface. While infestations persist, proper treatment of infected children can reduce the
harmful effects of these parasites. The study suggests that, at present, although
treatment of children with anti-worm medicine is common, children who had been recently
treated did not have a significantly lower prevalence of either infestation compared with
children who had never been treated. This was true regardless of sex, age, education of
parents and occupation of father. The most likely explanation for this is that medicine is
being used incorrectly - for example, the practice of sharing out bottles of anti-worm
medicine among children in a family is known to be common. This finding highlights the need for community education about the proper use of
available drugs and medicines. The option of organising general or targeted treatment
should also be considered. Chris Smith, Project Officer, UNICEF (West Bank and Gaza Strip), PO Box 141,
Shu'fat, East Jerusalem, Israel. This study was conducted by Birzeit Community Health Unit in co-operation with the
Gaza Red Crescent Society and the UN Relief and Works Agency. Comment
Should helminth infections be controlled by mass medication? William
Cutting offers one viewpoint. The germs that cause diarrhoea and the worms that are sometimes passed in stools both
live in the human gut. These infections are transmitted from the stools to the mouth - the
faecal-oral route. The most important preventive measures for both are therefore
improvements in water supply, sanitation and hygiene behaviour. Two of the parasites, Trichuris
trichuria and Strongyloides stercoralis. can cause watery, mucoid and even
bloody diarrhoea when infestations are heavy. Apart from these features, the infections are different in almost every way. Worms are
directly responsible for very few deaths, compared with the number caused by diarrhoea.
Mortality from roundworms (ascaris) may be 1 in 100,000 children infected, perhaps 13,000
in the world each year. Acute diarrhoea infections still kill almost 4 million children
each year, and have severe effects on the growth and development of many millions more.
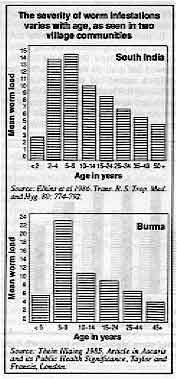 |
The severity of worm infestations varies with age, as seen in
two village communities
Sources:
Elkins et al 1986. Trans. R. S. Trop. Med and Hyg. 80: 774.792.
Thein Hlaing 1985. Article in Ascaris and its Public Health Significance, Taylor
and Francis, London.
Worm infestations are endemic in developing countries, mostly in children aged from
five to ten years (see table). However, levels of infestation vary enormously from place
to place. High levels are associated with poverty, poor sanitation and poor hygiene
practices.
|
Some major health agencies have recently focused on developing medication programmes
for controlling helminth parasite infections (1). They believe that with
three antiparasitic drugs (albendazole, praziquantel and ivermectin) it would be possible
to give mass treatment for most of the major human helminth infections. This treatment,
given once every year, could be combined with giving key nutrients, vitamin A in
particular. Doing this through the school system would reduce the costs to about $1 per
child per year, and it is believed that this approach would reduce malnutrition, ill
health, and the number of deaths: and improve growth, development and even intellectual
performance. Best use of resources Any campaign would thus be directed at school age children. However, in most developing
countries it is pre-school children who suffer most ill health. Among older children, it
is usually those who are not attending school who are in greatest need. This type of approach would have some serious consequences. Money spent on such a
programme might detract from investing resources in the development and strengthening of
primary health care systems and even basic health care services like the provision of
water supplies. WHO estimates that over two million child deaths every year could be
prevented by ORT - ensuring the right use of ORT has to remain a primary objective for
health services. A decision about including deworming in a child health programme should
be preceded by careful surveys to find out which children in the community are at risk of
infection, and therefore should be given medication. Preventive measures, which also help
to control the spread of diarrhoea infections, need to be given priority. Dr William Cutting, University of Edinburgh, 17 Hatton Place, Edinburgh EH9 1UW, UK.
1. Warren, KS. 1991. Helminths and health of school age children,
Lancet. 338: 686-7. Another viewpoint on this issue will follow in a future DD.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  6 Page 7 8 6 Page 7 8
| Questions and answers about ORT |
A child refusing to drink? Oral rehydration therapy may be easier in theory than in practice. What can be done in
the case of a child with dehydration from diarrhoea who cannot be persuaded to take ORS
solution, and where there are no facilities for IV treatment? Alhaji A B Amadu, The Zonal Health Management Committee Office, Lokoja General
Hospital, Lokoja, Nigeria.
Children with definite signs of dehydration are usually thirsty; they almost never
refuse to take ORS solution. The two most common explanations for refusal to take ORS
solution are (i) the child is not really dehydrated or
(ii) the child is too weak or lethargic to take the solution, as may occur when
dehydration is severe. In a few instances the cause is severe dehydration, and rehydration should be by the
intravenous route or, if this is not possible, by giving ORS through a nasogastric tube. Giving ORS solution takes patience and time, especially if a child is weak or drowsy. A
child is more likely to be persuaded to accept ORS solution from his or her mother, or
someone else known and trusted. Older children, who do not have signs of dehydration, may
refuse the solution because they do not like the taste. For such children, try adding a
little fruit juice, or give the ORS solution alternately with plain water or with another
familiar fluid that the child is more willing to drink.
Correct recipe for SSS? In my area there is some disagreement over how to make sugar-salt solution
(SSS) for
rehydration. Some doctors say that the recipe we promote (one pinch of salt to four
pinches of sugar) is wrong. This confuses health workers. Can DD help? Fr Emmanuel, Operation Health 2000, 32 College Road,
Nungambakkam, Madras 600 006,
India.
Teaching people how to measure out the correct amounts of salt and sugar to make home
made solutions is often a problem. The amount of sugar or salt in a finger pinch can vary
considerably, according to the individual's hand size and their judgement. People have
tried using teaspoons, but the size of these also varies. Some programmes have promoted
other standard-sized and locally available measuring devices (such as special plastic
spoons or fizzy drink bottle tops).
Studies show that people are more likely to make a solution that is more rather than
less concentrated than recommended. Solutions containing too much sugar and/or salt can be
dangerous, and may even increase the diarrhoea.
A child in danger of dehydration needs to be given fluids. It is better to give a child
as much as they will drink of a less concentrated solution than risk giving them too much
of one that may be dangerous.
Because of these problems, WHO now recommends the following quantities of salt and
sugar for home made SSS:
- 3g (half a level teaspoon) of salt and
- 18g (four level teaspoons) of sugar
- dissolved in one litre of clean drinking water.
WHO does not encourage the use of linger pinches or hand scoops to measure salt and
sugar for the reasons given above. The recipe used in Madras appears to provide too little
sugar, as one pinch (using the thumb and two fingers) equals about 0.5g of salt or sugar.
Thus, four pinches would provide only about 2g of sugar (per litre of water).
Alternatives to packets? Diarrhoea is a major problem in our area. We use ORS packets from UNICEF. But we have
not been able to teach people how to make their own oral rehydration solution because
sugar is not available locally. Salt can sometimes be found in a market which is four
hours' walk from us. People do have honey available. Can honey be used instead of sugar to make a home
solution for ORT? Are there any leaves that have enough natural sodium content that they
could be dried, crushed and added to the drink? Sharon Smith, Nurse Practitioner, Box 127, Addis Ababa, Ethiopia.
There are no widely used 'natural' substitutes for salt. Honey can be used as a substitute for glucose or sugar as 30 to 40 per cent of honey is
glucose. About 50ml of honey to a litre of water will provide the required amount of
glucose for a home solution. Cereal flour (such as rice, wheat, millet, sorghum or maize) can also be used instead
of sugar to make a home made solution. Cereals contain carbohydrates which are converted
into glucose in the intestine. Make this solution by adding two handfuls of flour to a litre of water. Boil, stirring
constantly, until the first bubbles appear (usually about five minutes), and then remove
from the heat. The solution should not be too thick to drink. After the mixture has
cooled, add two three-finger pinches of salt. If it is not possible to get ORS packets or to make home solutions with salt and sugar
or sugar substitutes, giving other types of fluids readily available in the home helps to
prevent dehydration. As well as plain water, these include vegetable and pulse based soups
and cooked cereal porridge.
Different formulations? Many families, especially in rural areas, do not think SSS and ORS solutions are
appropriate treatment for diarrhoea, as they believe that tablets, capsules and syrups are
the only 'real' treatment for illnesses. I suggest that WHO and other organisations should consider developing ORS in tablet or
syrup form, or making pills of the correct amount of sugar and salt which can be dissolved
in a specific amount of water, so that people are more convinced of their effectiveness.
What is your opinion about this'?
Bulama Abatcha, General Hospital Monguno, Monguno Local Government, Borno State,
Nigeria.
Medicines are usually bought, and given, in small quantities after a child has been
sick for a few days. If ORS is perceived as a medicine, to be bought in tablet form, there
is a danger that people will not give a child sufficient solution soon enough after
diarrhoea starts to prevent dehydration. Tablets and other formulations may also be more
expensive to produce, and therefore to buy, than ORS packets. It is important to teach people about the value of giving extra fluids, as well as
ORS solution and SSS, at home as soon as a child has passed the first loose stools. in
order to prevent dehydration. Oral rehydration therapy, in all its forms, enables families to take care of children
with diarrhoea themselves, without having to spend money on expensive drugs. However, ORS tablets (one tablet for 120ml, about one glassful, of water) are
commercially available. The product has been registered in many countries of Africa. Asia,
Central and Latin America and in the Middle East. For information contact: PATH (Program
for Appropriate Technology for Health), 1 Nickerson St., Seattle, Washington, 98109-1699,
USA.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 47 December
1991  7 Page 8 7 Page 8
ORT success in the Soviet Union ORT was first promoted widely in the Soviet Union for treating adults during cholera
outbreaks in Astrakhan (a region in southern Russia) in the early 1970s. But. until 1985,
the standard treatment for childhood diarrhoea was an intravenous drip. Doctors advised
withholding food to 'rest the bowel' and often prescribed antibiotics. Since 1985 the
Institute of Epidemiology, together with the health authorities, has set up ORT units in
city hospitals and local children's clinics, in rural hospitals and health facilities, and
they have also promoted home treatment. Health workers at different levels are being
trained, and TV and radio broadcasts used to educate health workers and parents about ORT.
|
Learning about oral rebydration at the ORT centre in one of
the hospitals in Astrakhan, Soviet Union.
Analbsis of 250 case reports from the Regional Infectious Clinical Hospital's ORT
Centre showed that most cases were . in children under a year old who were given
artificial milk alone or in combination with breastmilk. Four fifths of patients were .
treated at home with WHO formula ORS solution, and the vast majority recovered within two
or three days.
|
 |
An evaluation of the ORT centres after five years shows that:
- ORT is effective for in-patients;
- ORT units had been set up in all out-patient departments;
- hospital admissions for diarrhoea had decreased; and
- most mothers are aware of ORT and correct feeding practices.
But some actions are still needed:
- health workers and doctors need more training on ORT, as many of them are still using
intravenous drips unnecessarily, and on correctIy diagnosing the degree of dehydration;
paediatricians often use ORS onIy to prevent dehydration or during recovery, not to treat
dehydration;
- the supply of ORS packets should be improved to meet actual needs;
- the use of antibiotics, especially in rural areas, as a first-line treatment for acute
diarrhoea should be discouraged;
- breastfeeding should be more vigorously promoted.
Dr S Saroyants, Dr V Burkin, Dr G Dienko and Dr L
Chichkova, Institute of
Epidemiology, 416601, GSP, Astrakhan, USSR.
USA learns ORT lessons Diarrhoea is not just a cause of child death in developing countries. In the USA, 500
children under five die every year from diarrhoea - one every 18 hours. Many of these
deaths occur in poor communities with inadequate sanitation. More than 200,000 children
are taken to hospital with dehydrating diarrhoea every year. Intravenous therapy is the
standard treatment. This usually means several days in hospital, but in spite of this,
studies showed that half the children who died of diarrhoea did so in hospital. This may
have been because parents did not take the child to hospital soon enough or gave the child
inappropriate fluids at home. Most of these deaths could be prevented if oral rehydration therapy (ORT) were to 2 be
used. ORT has other advantages which are as relevant to the USA as to developing
countries:
- it is easy to give, at home as well as in hospital;
- it is inexpensive;
- it reduces the need for admission to hospital, thus reducing the costs to the national
health budget and to families.
Various organisations are co-operating to form the National ORT Project, to promote the
use of ORT in the USA. Dr Mathuram Santosham of Johns Hopkins University campaigned ten
years ago to promote ORT in a Native American Indian community in Arizona, USA, and child
diarrhoea mortality there was reduced to almost zero. He comments: 'We have been behind in
introducing this therapy. We ought to catch up with the developing world.' The cost in the USA of commercially available ORS, or ORT solutions (pre-mixed fluids).
is however very high. One litre costs between $4 and $6, and a dehydrated child usually
needs at least 4 litres. Reducing the cost would make promotion of ORT much easier. Johns
Hopkins Hospital has started to give people less expensive ORS packets based on the WHO
formula, and has found that these are acceptable to families and correctly mixed, if
proper education is given. Health staff resistance to using ORT quickly disappeared, when
they found that the time it takes to explain ORT to a family is far less than the 12 hours
or more needed to rehydrate a baby intravenously. Source: American Medical News, May 1991.
|
Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nel Druce DD thanks Hasan Shareef Ahmed (ICDDR,B) for help
with DD47 during his
stay at AHRTAG Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Dang Due Trach (Vietnam)
Professor Andrew Tomkins (UK) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 47 December 1991
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
updated: 23 August, 2019
|