|
| |
Issue no. 44 - March 1991
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
updated: 23 April, 2014
Pages 1-8 Dialogue on Diarrhoea Online Issue 44 -
March 1991
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 Page 1 2
Page 1 2
Anti-diarrhoeal drugs unmasked
Dialogue on Diarrhoea again stresses the dangers of the unnecessary or careless
use of drugs in the treatment of acute diarrhoea in children, in this third part of the
series 'Drugs and diarrhoea'. This issue looks at more of the anti-diarrhoeal medicines
which are widely advertised, sold over the counter and even prescribed throughout the
world. These drugs are expensive, dangerous and useless; poor families spend money they
cannot afford to do harm rather than good to their children. The World Health Organization
has now published its review of anti-diarrhoeal drugs (see="#page4">page 4 for
details). Not all drugs should be damned, however, and a future issue of the Dialogue will
discuss the correct way to use drugs to treat diarrhoea. Giving the right advice
In all countries more widespread education is needed about the importance of cheap and
simple oral rehydration therapy (ORT) as the first remedy (and often the only remedy
required) for acute diarrhoea. This crucial information must become commonplace thinking
at all levels of all societies and be backed up by all health professionals, including
pharmacists. The story on="#page6">page 6 shows how an ORT unit has saved money for a
hospital in Lesotho - more children can be treated effectively in the out-patient
department, before their illness becomes life-threatening. The article from Indonesia on="#page5">page 5 shows that all too often
doctors fail to give good advice about diarrhoea management. Many parents feel that their
child needs a drug to get better; doctors can help them to understand how oral rehydration
therapy and continued feeding can make the difference.
|
Continued breastfeeding is the best 'treatment' for an infant
with diarrhoea, as a reader points out in a letter on="#page7">page 7.
Breastmilk will help to prevent dehydration which can lead to death.
The picture on this page should remind everyone that breastfeeding protects babies and
young children against diarrhoeal infections: bottle-feeding can be very dangerous. Also in this issue, a special insert features shigellosis (or
bacillary dysentery), including information about causes, prevention and treatment of the
illness. Shigella infections are responsible for over 25 per cent of diarrhoea related
child deaths in some countries, many of which could be prevented by rapid diagnosis and
appropriate case management.
|
 |
|
In this issue:
- Anti-diarrhoeal drugs: not recommended
- Doctors still prescribe too many drugs for diarrhoea
- ORT saves money for a hospital
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 1 Page 2 3 1 Page 2 3
Adsorbents and sulphonamides
Adsorbents and sulphonamides are no longer recommended for treating acute
diarrhoea. This DD review, the last in the series, 'Drugs and diarrhoea', explains
why they are ineffective and sometimes dangerous. Kaolin and pectin
Although kaolin and/or pectin can improve stool consistency in some children with
acute diarrhoea, they do not appreciably reduce diarrhoea duration, stool frequency, or
stool losses. Their use may also detract from the most important treatment for diarrhoea -
ORT and continued feeding. Kaolin and pectin may also stop antibiotics working properly
when they are needed. Kaolin and pectin are not recommended for diarrhoea treatment. For
the same reasons, other adsorbents with similar properties (such as
attapulgite, smectite
and activated charcoal) are also not recommended. Formulations
Kaolin and pectin are often combined in a liquid preparation. They are marketed under a
variety of brand names, and are often sold in combination with antibiotics, vitamins, or
other drugs. Pharmacology
Kaolin is a naturally occurring clay, composed of hydrated aluminium silicate. It is
not absorbed when taken by mouth, and is excreted in the stool. Pectin is a carbohydrate
isolated from the peel of citrus fruits or green apples. Polygalacteronic acid, its main
constituent, is almost completely digested and absorbed in the intestine.
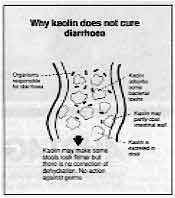 |
Why kaolin does not cure diarrhoea
- Organisms responsible for diarrhoea
- Kaolin absorbs some bacterial toxins
- Kaolin may partly coat intestinal wall
- Kaolin is excreted in stool
- Kaolin may make some stools look firmer but there is no correction of dehydration.
No action against germs
|
How they work
It has been claimed that kaolin adsorbs toxins, alters bacterial flora and can 'coat'
the intestinal lining to produce a 'general protective effect'. Kaolin appears to bind
cholera toxin, but not the heat-stable toxin of enterotoxigenic E. coli. It
does not appear to have any anti-bacterial action, nor is it able to 'adsorb' bacteria. Efficacy
Kaolin has been used as an anti-diarrhoeal agent for hundreds of years. Pectin became
popular with the use of 'apple powder diets' as a simple remedy for diarrhoea about 80
years ago. In animal studies, kaolin-pectin has been shown to: Extra fluid in bowel causes diarrhoea
- decrease toxin-induced intestinal secretion in pigs when injected into the bowel at the
same time as enterotoxigenic E. coli;
- reduce the volume of diarrhoea in dogs when given before or with cholera toxin, but not
after;
- improve stool consistency in monkeys with diarrhoea caused by cholera toxin.
But in a controlled clinical trial in 1970, kaolin was ineffective in cholera
treatment - with no effect on stool volume or diarrhoea duration. A study of 97
children with acute diarrhoea treated with kaolin or supportive therapy alone, showed no
difference in the duration of diarrhoea, mean number of stools per day, or the clinical
course of the disease. In another study, a kaolin-pectin combination given to children
with acute diarrhoea resulted in more 'formed' stools, but neither of the agents alone or
in combination made any difference to stool frequency or stool weight; thus the loss of
water and salts in the stools was not reduced. Adverse effects
A kaolin-pectin combination given to rats caused increased losses of sodium and
potassium in the stool. Kaolin-pectin might therefore worsen electrolyte disorders in
children with severe diarrhoea. Kaolin-pectin has also been shown to cause increased fat
and nitrogen losses in the stool.
 |
Some causes
of diarrhoea
Drug interactions
The effectiveness of some other drugs, such as
trimethoprim, chloroquine and pyremethamine, is reduced when they are given with kaolin-pectin. The interaction with
trimethoprim is important for diarrhoeal diseases management because
trimethoprim/
sulphamethoxazole (cotrimoxazole) is widely used for the treatment of Shigella dysentery.
Neomycin (an antibiotic which is not generally recommended) is bound by clays such as
kaolin in laboratory studies. Yet a large number of currently available 'anti-diarrhoeal'
compounds combine kaolin and neomycin. |
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 2 Page 3 4 2 Page 3 4
Other adsorbents Attapulgite and smectite
Attapulgite and smectite are mineral clays, similar to kaolin in composition, which are
not absorbed systemically. They are marketed as 'anti-diarrhoeal' drugs. Although they may
change the appearance and consistency of the stool (by adsorbing water from the bowel
cavity), there is no evidence that they reduce the loss of water and electrolytes from the
bowel in acute diarrhoea. Laboratory studies comparing the capacity of attapulgite and
smectite to adsorb different bacteria have shown varying results. A number of clinical trials have evaluated smectite as an adjunct to ORS for the
treatment of diarrhoea in children. However, only one controlled study has been conducted,
in Egypt, where smectite or a placebo was given to 90 hospitalised children under three,
in addition to ORS. It showed no difference in total diarrhoea stool output, but the
duration of diarrhoea, from the time of hospital admission, was significantly reduced in
the smectite-treated group (54 hours) compared with the placebo group (73 hours). Smectite
appears to have little effect on stool output during the early, high purging phase of
acute diarrhoea, but can alter the stool consistency and frequency as the acute attack
wanes and intestinal transit time increases. This has, however, little value in the
routine management of acute diarrhoea.
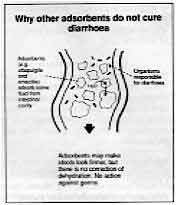 |
Why other adsorbents do not cure diarrhoea - Adsorbents (e.g. attapulgite and smectite) absorb some fluid from intestinal
cavity
- Organisms responsible for diarrhoea
- Adsorbents may make stools look firmer, but there is no correction of dehydration.
No action against germs
|
Activated charcoal
Adsorbent qualities of activated charcoal make it an effective antidote in the
emergency treatment of poisoning and drug overdoses. Activated charcoal is a black powder
sold in tablet or powder forms, sometimes in combination with antimotility drugs and/or
antacids. It adsorbs and inactivates a number of organic and inorganic compounds by
binding them in the gut. But there is no clinical evidence that it shortens diarrhoea
duration or reduces the number or volume of stools. Like other adsorbents, it also binds
to and makes other drugs such as tetracycline inactive, and affects digestive enzymes and
intestinal micronutrients. Sulphonamides
Non-absorbable sulphonamides (such as sulphaguanidine, succinylsulphathiazole, and
phthalylsulphathiazole) were once considered the drugs of choice in the treatment of
Shigella dysentery and other bacterial intestinal infections. They are still widely used
in some places, even though they have been shown to be ineffective and toxic, and many
bacteria have become resistant to them. There is no justification for their continued use,
and their distribution and sale has been banned in several countries. Formulations
Non-absorbable sulphonamides are marketed as a treatment for intestinal infections,
particularly bacillary dysentery (i. e. shigellosis). They are either sold alone or in
combination with other drugs. Pharmacology
All sulphonamides have the same antimicrobial spectrum; they differ only in how they
are absorbed, metabolised and excreted by the body. Non-absorbable sulphonamides work mainly in the large intestine. Absorption of
sulphaguanidine by the body is slow and erratic. Fifteen to 50 per cent is systematically
absorbed and excreted by the kidneys. About 5 per cent of succinylsulphathiazole and
phthalylsulphathiazole is systematically absorbed. The drug is mostly excreted in the
stools.
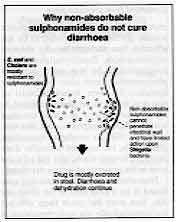 |
Why
non-absorbable sulphonamides do not cure diarrhoea - E. coli and cholera are mostly resistant to sulphonamides
- Non absorbable sulphonamides cannot penetrate intestinal wall and have limited
action upon Shigella bacteria
- Drug is mostly excreted in stool. Diarrhoea and dehydration continue
|
How they work
Sulphonamides stop or slow the growth of bacteria and are effective against many Gram
positive and Gram negative organisms. Absorbable sulphonamides (such as sulphadimidine and
sulphadiazine) have been shown to have some advantages against organisms that invade the
gut wall, like Shigella, that cause dysentery. Although the bacterial count of sensitive
organisms in the bowel is reduced in patients taking a non-absorbable
sulphonamide, the
stool never becomes sterile, and bacterial counts return to previous levels soon after the
drug is discontinued. In addition, bacterial resistance has greatly reduced the therapeutic range of the
sulphonamides - and since all sulphonamides work in the same way, bacteria resistant to
one are resistant to them all. Some bacteria are naturally resistant to
sulphonamides;
others have become resistant (see="dd42.htm">DD42). Bacteria that are
sensitive to sulphonamides can become resistant during the course of treatment. Most
Shigella strains are now resistant to sulphonamides. Resistant strains of E. coli and
other Enterobactericiae are also now common, particularly in hospitals.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 3 Page 4 5 3 Page 4 5
Efficacy
Bacillary dysentery
Non-absorbable sulphonamides were developed as a way of getting a large concentration of
the drug to the bowel, and avoiding the toxic effects of the earlier
sulphonamides. In the
194Os, before modem antibiotics were available, non-absorbable sulphonamides were
considered ideal for treating bacillary dysentery and other diarrhoeal illnesses. A
six-year field study of non-absorbable and systemically absorbed sulphonamides used to
treat bacillary dysentery in the USA reported that all sulpha drugs were effective when
compared with untreated controls; but the response to the systemically absorbed
sulphonamides was more rapid.
Sulphaguanidine was the first sulphonamide used to treat Shigella dysentery. Studies
suggested it was a promising drug that brought quick clinical results, but later it was
found to be less effective than the systemically absorbed sulphonamides.
Succinylsulphathiazole, considered to be less toxic than sulphaguanidine, was also used to
treat dysentery. However, its anti-bacterial action was found to be greatly reduced by
watery diarrhoea or ulcerated intestinal mucosa. Phthalylsulphathiazole, first used in man
in 1942, is similar to succinylsulphathiazole, but required a smaller dose, produced
formed stools, and was effective even in the presence of watery diarrhoea.
Non-absorbable sulphonamides continued to be widely used in the 1940s and 50s. But over
the years their efficacy declined markedly, due to the emergence of resistant strains of
bacteria. We now know that they have limited efficacy and potential toxicity. Importation
and/or production of sulphaguanidine has been banned in several countries. In the USA
sulphathiazole - the active ingredient in succinylsulphathiazole and
phthalylsulphathiazole - has been banned
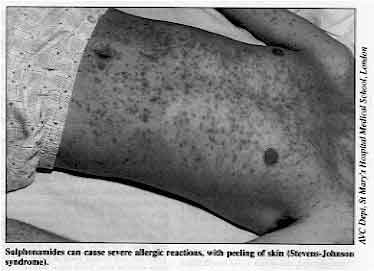
Sulphonamides can cause severe allergic reactions, with
peeling of skin (Stevens-Johnson syndrome)
|
 |
- Cholera
Although Vibrio cholerae is sensitive to sulphonamides in laboratory
experiments, non-absorbable and systemically absorbed sulphonamides have been proved to be
ineffective in the treatment of cholera. One controlled study of children and adults
hospitalised with cholera showed no difference in the duration of Vibrio cholerae excretion
between those treated with sulphonamides and the control groups. Kidney problems probably
contributed to the higher death rate found in the group treated with
sulphonamides.
Another controlled study compared the efficacy of chloramphenicol, tetracycline and
sulphaguanidine in patients with cholera. Sulphaguanidine had no significant effect on the
volume of diarrhoeal stool or the duration of Vibrio excretion.
Adverse effects Adverse effects of sulphonamides can affect nearly every organ system in the body. Rash
and fever, such as the Stevens-Johnson syndrome, are the most common side effects. More
rarely, sulphonamides affect the bone marrow and blood forming organs, the liver and
kidneys. In dehydrated patients, crystals of sulphonamide can form in the kidneys and
cause serious damage. Though less of the drug is absorbed, non-absorbable sulphonamides
are just as toxic as systemically absorbed sulphonamides. Destruction of the red blood cells caused by sulphonamides can lead to
anaemia, and
damage to the tissues which make white blood cells has also been reported Sulphonamides
can also cause jaundice if given to premature or newborn infants or to pregnant women. By
altering the bowel flora, non-absorbable sulphonamides may also interfere with the
bacterial production of vitamins. Drug interactions Sulphonamides may inhibit the effects of other drugs such as warfarin anti-coagulants,
anti-diabetic sulphonylureas, and hydantoin anti-convulsant. Adjustment of the doses of
these drugs may be necessary if they are given with sulphonamides. References for the studies referred to in these reviews are available from
DD/AHRTAG
and CDD/WHO. Diagrams supplied by Dr William Cutting
Drugs and diarrhoea: book review The drugs article in this issue of DD concludes the series on 'Drugs and
diarrhoea' (DD42,="dd43.htm">43,="dd44.htm">44).
The material used for the articles has been taken from a new book, The rational use of
drugs in the management of acute diarrhoea in children, just published
by the World Health Organization. The book provides information essential to those concerned with improving the rational
use of drugs in the treatment of diarrhoea. A body of research backs up the powerful
arguments against the widespread use of medicines which may harm a patient, and delay or
replace effective treatment measures. The use of anti-diarrhoeals and anti-emetics is often dangerous: critical evaluations
summarise the data on commonly-used drugs of this type. The book concludes that the
continued production, promotion and sale of these preparations for paediatric practice
cannot be justified. There is a limited number of drugs which are judged to be effective, and therefore are
recommended for the management of cases of diarrhoea where the cause has been diagnosed.
They are summarised in a table which lists first - choice antimicrobials, followed by
alternatives, for cholera, Shigella dysentery, amoebiasis and giardiasis. The rational use of drugs in the management of acute diarrhoea in children. WHO,
Geneva, 1990. 71pp, ISBN 92 4 156142 4. Available in English, French and Spanish from WHO
outlets internationally, and WHO Distribution and Sales, 1211 Geneva 27, Switzerland.
Price approx. US$ 9.90 to developed countries, US$ 6.95 to developing countries. Order no.
1150355.
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 4 Page 5 6 4 Page 5 6
To feed or not to feed?
DD reports on a study in Indonesia which found that although most doctors
knew they should advise parents to continue feeding during diarrhoea, in practice many
prescribed inappropriate treatments. The adverse effects of acute diarrhoea include both dehydration, due to the loss of
water and salts, and malnutrition, due largely to reduced intake of food. Physicians have
been encouraged by WHO and national CDD programmes to motivate mothers to continue
breastfeeding or giving other food to prevent malnutrition resulting from diarrhoea. The Atma Jaya Medical Faculty research group looked at the treatment and advice given
by physicians for children with acute diarrhoea in a poor and densely populated urban area
of Jakarta (the capital city of Indonesia). Over 100 physicians were interviewed, and 73
of them, (who were seeing more than ten children per week), agreed to allow their clinical
practices to be observed.
 |
Doctors should give parents advice about continued
feeding/giving fluids to a child with diarrhoea, as well as information about ORT. These physicians were working in private practices as well as in public institutions,
such as government health centres or hospital out-patient clinics.
|
Reported and observed practice on nutritional advice given to parents was
analysed, as
well as drugs prescribed and whether or not ORS was recommended. The study found that
although physicians believe that giving nutritional advice is part of good medical
practice in treating children with acute diarrhoea, they do not always offer nutritional
advice to parents in their clinical work (see="#Prescribing">Table). Differences in practice and belief
Only 7 per cent of physicians interviewed said they recommended 'resting the gut' in
treatment for acute childhood diarrhoea, and in only five of the 186 observed cases was
such treatment recommended. There was, however, a significant difference between belief
and practice related to giving nutritional advice and other treatments. In public health
centres and private practices, over 85 per cent of physicians said they gave nutritional
advice to parents; and 92 per cent said they believed that breastfeeding should be
encouraged when a child has diarrhoea. Yet, observation found that in only 53 per cent of
the 186 cases did physicians recommend any nutritional action, either continuing
breastfeeding or giving other foods. What explains the difference between what physicians believe to be appropriate practice
and what they actually do in their clinical work? There was a significant difference
between doctors in public and private practice. It is possible that physicians have more
time to give nutritional advice in their private practices than in public health centres. Prescribing medicines
The="#Prescribing">table also shows that physicians in both public and
private practice prescribed some form of medication, especially antibiotics, for a high
proportion of cases, and that medication was recommended more often than ORS. However,
doctors in the public sector prescribed ORS in many more cases, due possibly to effective
government information and training programmes. Physicians in private practice may feel
more obliged to meet parental expectations for a medicine that would help their children
to recover rapidly. This, and the tendency to focus on concerns about disease pathology
(the organism causing the diarrhoea) in both sectors, may lead to an emphasis on
medication rather than on nutritional advice. Nutritional advice was given less frequently
than antibiotics. These findings emphasise the continuing need to educate physicians about the
appropriate use of antibiotics and ORS, and the importance of giving correct nutritional
advice for children with acute diarrhoea.
Prescribing
practices of 73 doctors in the treatment of
diarrhoea |
Treatment |
Public |
Private |
Total |
| Nutritional advice |
41% |
67% |
99 cases |
| Antibiotics |
94% |
86% |
106 cases |
| Spasmolytics (spasm relieving drugs) |
31% |
30% |
61 cases |
| Adsorbents |
14% |
25% |
39 cases |
| ORS |
59% |
38% |
87 cases |
Herawati Arif and Lusia Gani, Department of Public Health, Atma Jaya Medical
Faculty, Jendrai Sudirman 51, Jakarta, Indonesia. With support from ADDR.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 5 Page 6 7 5 Page 6 7
| Reports from the journals |
Is oral rehydration therapy cost effective?
Although diarrhoeal disease control (CDD) programmes are widely perceived to be cost
effective, there is little documented evidence to support this. Those studies which do
show the cost effectiveness of CDD programmes need to be made more widely available to
strengthen the case for funding such programmes. This study describes the economic
benefits of establishing an Oral Rehydration Therapy Unit (ORTU) in a major hospital in
Lesotho. The ORTU was set up in February 1986 at the Queen Elizabeth II (QEII) Hospital in
Maseru. It provides case management for children presenting with diarrhoea to the
out-patient department: over 4,000 children under five years of age were treated during
the first two years. To evaluate the ORTU, a study compared the cost of treating
diarrhoeal disease at the hospital one year before the establishment of the ORTU (1985)
and one year after it was set up (1987). Treatment costs reduced
The cost per child under five years for treatment of diarrhoea was (including
in-patients and out-patients) 38 per cent less in 1987 than in 1985. Most of the saving
came from treating a greater proportion of diarrhoea cases as out-patients, rather than as
in-patients. In 1985, 12 per cent of children under five with diarrhoea were treated as
in-patients, compared with only 6 per cent in 1987.
Figure 2: ORTU savings in the first three years of
operation (1985-87) |
| |
M (Maloti) (1) |
| Total ORTU savings (from reduced admissions) |
36,166 |
| Total ORTU costs |
|
| Set-up costs: 8,000
|
|
| Running costs: 2,270
|
10,270 (2) |
| Net saving |
25,896 |
| 1. The local currency unit. In 1987, US$ l.00 = M2.4. |
|
| 2. Does not include costs of personnel already accounted for in hospital
budget for training of ORTU staff. |
The difference in cost between out-patient and in-patient treatment
reflects a decrease by half in the average cost of drugs and supplies for out-patient
diarrhoea treatment. Before the establishment of the ORTU, children with diarrhoea were
more likely to be treated with antibiotics than with less expensive ORS. After the ORTU
was established, they were likely to be given antibiotics in addition to ORS only if
admitted for treatment when the ORTU was closed. Most (67 per cent) children with
diarrhoea were treated in the ORTU with ORS only. Hospital admissions down
The number of diarrhoea related admissions to the paediatric ward decreased from 376 in
1985 to 218 in 1987 as shown in Figure 1. Admissions were split into 'complicated' and
'uncomplicated' categories. 'Uncomplicated' admissions were those for which diarrhoea or
gastroenteritis was the only diagnosis.
 |
Figure 1: Number of diarrhoea admissions to paediatric ward,
QEII Hospital, Maseru, Lesotho, 1985 and 1987
Children with diarrhoea plus another diagnosis were classified as 'complicated'
admissions; these made up about one fifth of total admissions. The cost per
'uncomplicated' admission was lower in 1987 than in 1985. The decrease was mainly due to a
reduction in the average length of stay from 5.7 days to 3.4 days, but also to a decrease
in the average cost of drugs per patient.
|
Costs per 'complicated' admission more than doubled between 1985 and 1987, but the
reduction in the number of such admissions led to an overall saving. On balance, the
reduction in admissions to the hospital, due to the work of the ORTU, led to total savings
of over US$ l5,000 (at 1987 exchange rates). The overall cost for treating diarrhoea cases in under fives was 1.3 per cent of the
total hospital expenditure in 1985, but only 0.57 per cent in 1987. Conclusion
Comparison of expenditure on establishing and running the ORTU for one year with the
savings due to the decrease in admissions shows a substantial net gain to the hospital,
and hence the cost effectiveness of the ORTU (Figure 2). This saving should be even
greater in subsequent years because set-up costs will not be required. This study shows
the usefulness of applying cost effectiveness techniques; in Lesotho they have highlighted
the contribution made by the CDD programme through appropriate case management. Diarrhoeal Diseases Control Programme, WHO, Lesotho. Weekly
Epid. Record No 36:
Sept. 1990. Cereal based ORT: pros and cons
Sucrose based oral rehydration therapy (ORT) for diarrhoea is promoted in many
countries. The Bangladesh Rural Advancement Committee (BRAC) programme has taught more
than 13 million mothers about a home based sugar-salt solution (SSS), and achieved very
high levels of knowledge about ORT and correct mixing. However, these women have
subsequently used SSS in only 20 per cent of all diarrhoea episodes. Mothers often complain that SSS does not stop diarrhoea. Since recent research has
shown that a rice based solution may decrease fluid losses, a BRAC study tested its
acceptability and use compared with SSS. Rice is more available in rural homes (95 per
cent) than all kinds of sugar (less than 30 per cent) and rice gruel is a widely accepted
food during illness. A field trial was conducted in early 1987 in three areas (total population 68,345).
Mothers were taught to make both types of solution through initial and follow-up
house-to-house visits by BRAC health trainers. Further follow-up visits (to a 5 per cent
random sample) were made at three monthly intervals for one year, to assess knowledge and
analyse the content of the solutions prepared. Focus group discussions were also held with
small groups of mothers to find out their opinions about the two types of ORT fluids. Although mothers unanimously recommended the rice based solution, because they thought
that this 'stopped' the diarrhoea more quickly, they used SSS twice as often (in 40 per
cent of severe watery episodes) as the rice based solution (18 per cent of severe watery
episodes). They found rice based solution more time consuming and difficult to prepare.
There was no significant difference in the proportion of the two solutions prepared with a
safe composition. Children also preferred the sweeter taste of the sugar-salt solution. In
addition, there are cultural barriers to giving 'solids' to children aged less than six
months old, as mothers believe that young infants cannot digest them, and rice is
considered a solid. In some areas lack of firewood is also a problem, preventing mothers
from preparing the rice based solution. In conclusion, convenience factor seemed to outweigh maternal preference when it came
to choosing the type of solution to use. These factors led to lower use rates of the
home-made rice based fluid, making it a poor substitute for SSS at community level in
rural Bangladesh. Chowdhury, A, et al., 1990. Home made oral rehydration therapy: a community trial
comparing the acceptability of sucrose and cereal base solutions. BRAC, 66 Mohakhali
Commercial Area, Dhaka 1212, Bangladesh.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 6 Page 7 8 6 Page 7 8
Appropriate drug marketing
MaLAM (the Medical Lobby for Appropriate Marketing) is an international group of health
workers promoting rational use through campaigning for improved drug marketing. The group
also provides information on medicine marketing through its monthly newsletter. Peter Mansfield, MaLAM, 22 Renaissance Arc, Adelaide, SA 5000, Australia.
Is industrial salt safe for ORT?
In Nigeria recently there has been a great scarcity of many household goods, including
salt. Industrial salt from factories was the only salt available for cooking, giving a
very salty taste to food, even when very little was used. What amount of industrial salt
should be used to make sugar-salt solution for ORT? Is it different from ordinary salt,
and is it dangerous? Ariyo Olusegun Raphael, P 0 Box 420, Ilorin, Kwara State, Nigeria.
Hans Faust of WHO replies:
Provided that the industrial salt mentioned is sodium chloride, it can be assumed that
it is more purified and cleaner than the usual household salt; it may also be fortified
with fluoride or iodine. This may explain why the taste seems stronger than that of
household salt. The amount of industrial salt to use is the same as for other types of
salt -3 grams per litre of water.
|
Household or industrial salt can he safely used for making
sugar-salt solution. However, the volume of salt required to make 3 grams varies according to the size of
the crystals. Fine crystals pack more closely and require a smaller volume; large crystals
do not pack as closely and need a larger volume. For this reason it should be determined
whether one level teaspoonful (using a local standard teaspoon) of industrial salt weighs
about 3 grams. If the weight is much more than this, i. e. 4.5 grams or more, another
means of measuring the salt should be sought.
|
 |
Ethiopia: local beliefs about nutrition
In DD41, I was interested to read the letter about local beliefs and diarrhoea.
I work as a nutritionist in Western Ethiopia, and have been collecting information about
local beliefs. Many people do not know what causes diarrhoea, although some know that
dirty water or the ascaris worm can be the reason. However people also believe that the following can cause diarrhoea: teething in small
children; a bad fall; eating 'germinated flour'. During diarrhoea, people commonly believe
that food and drink should not be given, in order to 'dry out' the diarrhoea. Many feel
that if the person wants to drink more, he or she will soon die. Local foods recommended
for 'curing' diarrhoea include dry bread mixed with soot; honey mixed with instant coffee
powder; roasted niger seed - none of which is appropriate. Many of these local beliefs are very dangerous, and we are designing teaching aids and
handouts to try to discourage them and encourage good practice. Veronika Scherbaum, Nejo Clinic, EECMY, Nejo, Wollega Province, Ethiopia.
Value of breastfeeding during diarrhoea
We still need to correct the wrong impressions some mothers have that breastmilk
worsens diarrhoea. Breastfeeding is the best food during diarrhoea. Apart from helping to
prevent dehydration, breastfeeding is beneficial during and after diarrhoea. Constant
breastfeeding during diarrhoea shortens its duration. It also reduces nutritional losses
which usually accompany diarrhoea. The consumption of breastmilk during diarrhoea is
maintained while that of other foods is often reduced. Infants often continue with
breastmilk while refusing other foods, especially non-human milk, during diarrhoea. Adewole Atanda, Environmental Health Officer, Oyo Local Government, PMB 1008, Oyo,
Nigeria.
Local distribution of DD DD in English is free to readers in developing countries from the address in the
UK on the back page. But did you know that you can get DD in other countries
as well? The following organisations will be able to send you free copies in the language
indicated: Bangla: BRAC, 66 Mohakhali C A, Dhaka -12, Bangladesh; and Child in Need
Institute (CINI), P O Box 16742, Calcutta 700072, West Bengal, India
Chinese: Paediatric Section, Foreign Medicine Editorial Dept., China Medical
University, 3rd Affiliated Hospital, No. 6, Section 1, Sanhao St, Shenyang,
Liaoning, P R
China
French: ORANA, B P 2089, Dakar, Senegal
Nepali: HLMP, Institute of Medicine, Tribhuvan University, P O Box 2533,
Kathmandu, Nepal
Portuguese (in Mozambique and Angola only): Ricardo Barradas and Ana
Novoa, Faculadade de Medicina, Universidade E Mondlane, C P 257, Maputo, Mozambique
Spanish: Grupo CID, P 0 Box 39256, Washington DC 20016, USA
Tamil: RUHSA, Christian Medical College and Hospital, RUHSA Campus, P O 632209,
North Arcot District, Tamil Nadu, India
English editions are also available in country from:
India: CMAI, Plot 2, A-3 Local Shopping Centre,
Janakpuri, New Delhi 110058
Pakistan: Imajics (Pvt Ltd), F-25/ A, Block 9, Clifton, Karachi
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 44 March 1991
 7 Page 8 7 Page 8
ORS - given too late in diarrhoea treatment
It is unfortunate to note that many families view sugar-salt solution
(SSS) and ORS
solution as 'medicine' and so give them too late, as mentioned in DD42.I assume that this is one of the results of social marketing programmes used to
promote ORS, especially when ORS is sold in pharmacies and mothers know that only drugs or
medicines are sold there. With education which emphasises not using drugs unnecessarily,
no mother likes to apply a 'drug' to a case of diarrhoea until it has progressed to a
severe stage. This is what I have found in interviews with some mothers attending our MCH
centres. I suggest that programmes marketing and distributing ORS should be reviewed to take
account of these issues. Anthony E Koomson, Nutritionist, ADRA, P O Box 1435, Accra, Ghana.
More ideas for nutritious weaning foods
In DO40 weaning foods were discussed. I would like
to describe the type of weaning food used here. Our Community Health Post is in the rural
area around Ilorin and the weaning food developed and taught by community health workers
to mothers is called 'soya-ogi'. This contains soy beans and porridge (of maize or guinea
corn). This mixture, apart from being readily available, is also cheap. Mothers are
encouraged to include processed soy bean in their children's porridge (porridge being the
usual weaning diet). It ensures that much-needed protein is present in the diet of the
child, thus helping to reduce death from malnutrition. The soy beans are processed by boiling them in water for 15 to 20 minutes, to soften
the coat and allow its easy removal. After removing the coat, they are boiled again for
another 30 minutes to remove the unpleasant smell usually associated with soy beans. After
drying in the sun, the beans are slightly roasted and turned into powder (flour) by
grinding or milling. This flour can be stored in a clean, dry, closed container. The
preparation can be kept for up to three months without spoiling. The 'soya-ogi' is prepared by boiling three cupfuls of water in a pot with one
teaspoonful of palm oil added. Two heaped teaspoonfuls of the processed soy bean flour are
added next and the mixture is boiled again before adding ogi (fermented maize or guinea
corn porridge) to make a thick mixture. Sugar is added last to taste. Mothers are
encouraged to give the meal with a cup and spoon and advised to discard any left over
after 24 hours. Apart from its use as a weaning food, it is also given during diarrhoea in addition to
SSS, which is used commonly here. Salami Taofik, Faculty of Health Sciences, University of
Ilorin, Ilorin, Kwara
State, Nigeria.
A cautionary tale: dysentery
Recently my daughter, aged 17, had severe vomiting, diarrhoea and a fever. The doctor
told her to stop eating altogether and drink nothing but Coca-Cola. "You must rest
the gut," he said, "and don't feed the germs." She got very hungry and even
weaker. She couldn't drink a lot of Coca-Cola - it was too sweet. The diarrhoea stopped after two days so it was difficult to provide a stool sample for
analysis. Eventually she produced a few drops of bloody mucus. A week after first seeing
the doctor a diagnosis was made - shigellosis (caught in Romania). She was still suffering
from intermittent fever, was by now very weak and had lost nearly eight kilos. She was
prescribed a course of antibiotics. Was the doctor correct in saying "Don't eat - starve the germs"? Would there
be more or less bleeding and inflammation if food were eaten? Janie Hampton, 118 Hurst Street, Oxford, UK.
Dr William Cutting replies:
Janie Hampton's story of her daughter's diarrhoea is salutary. The fact that her
daughter had both fever and blood in her stools should have alerted the doctor to the fact
that this was not simple diarrhoea but dysentery.
- Drinks are the right way to treat virtually all cases of diarrhoea, but the sort of
drink is important. Coca-Cola is mostly sugar in water and contains very few salts which
are most important. The sweetness even put Janie's daughter off the most important aspect
of the treatment, drinking.
- Food is an important part of the treatment. "Rest the bowel" is an old
fashioned idea. It is now known that recovery is faster if, once the fluid has been
replaced, food is taken by mouth, as the nourishment of the cells of the lining of the
bowel depend on this. Starving will just cause additional harm to the bowel, and the
patient will lose weight.
- Antibiotic drugs have a definite but limited place in the treatment of diarrhoea.
Janie's daughter had specific indications for an antibiotic - dysentery stools containing
blood, and fever, suggesting that she had germs that were invading and damaging the bowel
wall. Appropriate treatment could have been with ampicillin or
cotrimoxazole.
Even in a home with modem water supply and hygiene facilities, diarrhoea is contagious
and extra precautions should be taken to avoid other members of the family getting the
disease. These are mainly simple things like handwashing after using the toilet, after
handling soiled nappies and clothes, and especially before preparing and eating food.
Shigella dysentery is particularly contagious, as only a few germs are needed to cause the
infection. (See="su44.htm">insert on Shigella in this issue.)
|
| Next issue DD45 will cover diarrhoeal problems in
refugee camps and cholera. |
Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nel Druce
Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Nicole Guérin (France)
Dr Norbert Hirschhorn (USA)
Dr Sharon Huttly (UK)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 44 March 1991
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 April, 2014
updated: 23 April, 2014
|