|
| |
Issue no. 11 - November 1982
pdf
 version of this Issue version of this Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Diarrhoea Dialogue Online Issue 11 -
November 1982
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  Page 1 2
Page 1 2
Control programmes:
the key role of laboratories
Oral rehydration therapy (ORT), properly given, is always the first-line treatment for
diarrhoea. Nevertheless, there is only one effective way to control this problem. The
causes must be identified and the sources of infection traced and treated within
communities. Advances in techniques Until recently control programmes have been handicapped because, up to ten years ago,
the exact cause of diarrhoea could only be established in 15-20 per cent of cases. Thanks
to advances in laboratory techniques, an accurate diagnosis can now be made for at least
80 per cent of those who attend treatment centres which have access to appropriate
laboratory facilities.
|
Laboratory workers in Ethiopia
Different levels of investigation play a crucial role both in the treatment of
individuals and in national control programmes. Knowing what organisms are causing
diarrhoea makes surveillance easier. Epidemics and unusual infections can be spotted early
and prompt warning given of the possible emergence of drug resistance among local strains
of pathogens. Specific interventions can be more effectively planned, implemented and
evaluated.
|
 |
Good management
Success in planning and implementing diarrhoeal disease control programmes depends on
good management at all levels. The World Health Organization is already providing senior
management training courses for planners of national diarrhoeal disease control
programmes. It is WHO's intention in the near future to offer appropriate management
training to middle level health care personnel who will be responsible for the supervision
of programmes in the field. In this issue of Diarrhoea Dialogue, we look at some of the key points
which health workers need to know about collection and transport of faecal specimens. The
practical advice page describes simple, screening procedures which can be undertaken at
any health centre possessing minimal equipment. At this level it is possible to make two
important distinctions; between secretory and invasive diarrhoea (dysentery); and between
bacillary and parasitic dysentery. These distinctions are very useful guides in
decision-making about the immediate treatment of individual patients. Targetting control measures
In all investigations, the closest collaboration must be ensured between clinical
personnel, epidemiologists and microbiologists. Good epidemiological and clinical
information speeds up and improves laboratory analysis of specimens. Similarly, the
increased capability of laboratories to feed back an accurate diagnosis to the field
permits more effective targetting of appropriate control measures. The complexity of the
investigation that can be carried out in any particular situation obviously depends on the
level of equipment and technical expertise that is available. A carefully planned and
efficient network of laboratory services is thus a valuable component in any country's
diarrhoeal disease control strategy. K.M.E. and W.A.M.C.
|
In this issue...
- Basic laboratory techniques
- Reviews of laboratory manuals
- Health education and diarrhoeal diseases
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  1 Page 2 3 1 Page 2 3
Success through education
The development, production and use of health education materials should be a major
concern at all levels of diarrhoeal disease control programmes.* We have heard
recently of various initiatives in this area. Jamaican materials
The Jamaican Ministry of Health and the Caribbean Food and Nutrition Institute have
recently produced a set of teaching materials, funded by the WHO diarrhoeal disease
control programme. The set contains:
- booklets with line drawings and photographs to tell mothers what to do when their
children have diarrhoea and how they can recognize the signs and symptoms of dehydration.
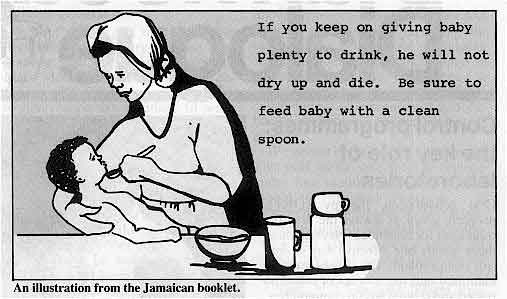
An illustration from the Jamaican booklet.
- a manual for health workers containing technical information on diarrhoea and ideas on
various ways that can be used to communicate messages to mothers
- a poster showing the signs and symptoms of dehydration to reinforce the message being
put across by the health workers.
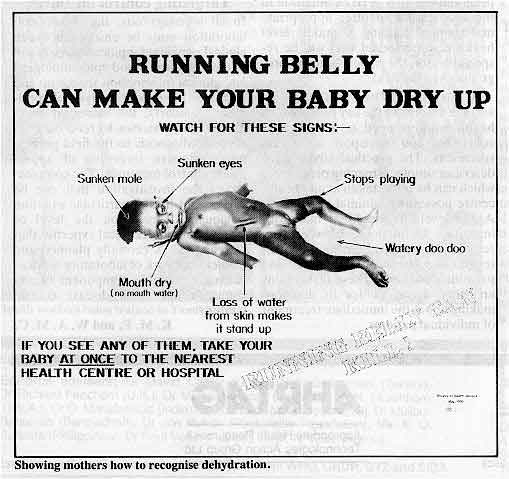
Showing mothers how to recognise dehydration.
For more information about these materials contact: Elizabeth Grant, Field Co-Ordinator
for Programme for the Control of Diarrhoea in Jamaica, Ministry of Health, 10 Caledonia
Avenue, Kingston 5, Jamaica. Poster sets
Solange Muller has written to tell us about some poster sets being used in Nicaragua.
The materials have also been tested in Mexico, the Dominican Republic and Honduras. The
sets consist of two large posters (30cms x 40cms) one showing a thin dehydrated child and
the other a healthy child, and at least ten small cards (15cms x 10cms) showing the causes
of diarrhoea and ways of preventing it as related to conditions in that particular
country. The small cards show simple line drawings of:
- a child defaecating outside
- a hand with dirty nails
- a baby bottle with flies on it
- a latrine
- food covered with a cloth
- a mother breastfeeding
- a mother giving oral rehydration solution.
If a large number of posters and cards are being made, they can be silk screened. But
usually the health workers can make the materials themselves, by tracing from an original
set and then colouring them in. When using the posters, health workers should:
- show the mothers the poster of the thin dehydrated child
- ask for their comments
- ask whether there are any children in the community like this and why they get this way.
If mothers have problems in recognizing that the child is dehydrated because of
diarrhoea. the health worker can give suggestions. The main idea is to encourage mothers
to share ideas on diarrhoea. Each mother then selects one of the small cards, explains what the drawing means to her
and puts the card next to one of the two large posters, explaining why the card goes with
the poster. After this, the mothers discuss with the health worker what they have learnt
about preventing diarrhoea. The set of posters and cards has been developed by Solange Muller and Felipe Orrego in
the Dominican Republic for the Save the Children Fund, USA. For more information contact:
Solange Muller, Apartado A-51, Managua, Nicaragua.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  2 Page 3 4 2 Page 3 4
Brazilian workshop
The Pan American Health Organization (PAHO) and the Centro Americane para Tecnologia de
Education de Salud are organizing a workshop in Rio de Janeiro in December 1982.
Participants will consider different ways of developing communications support for
diarrhoeal disease programmes and produce some materials for field testing. There will be
a report on the workshop in Diarrhoea Dialogue 12. WHO catalogue
The diarrhoeal disease control programme of WHO, Geneva is developing a catalogue of
health education materials on the causes and prevention of diarrhoea. The catalogue shows
posters, leaflets, journals and newsletters from all over the world. It will be available
from WHO early in 1983. For more information contact: the Programme Manager, Diarrhoeal
Disease Control Programme, World Health Organization, 1211 Geneva 27, Switzerland. *="dd09.htm">Issue nine of Diarrhoea Dialogue gave a list of
organizations who can supply information on health education materials.
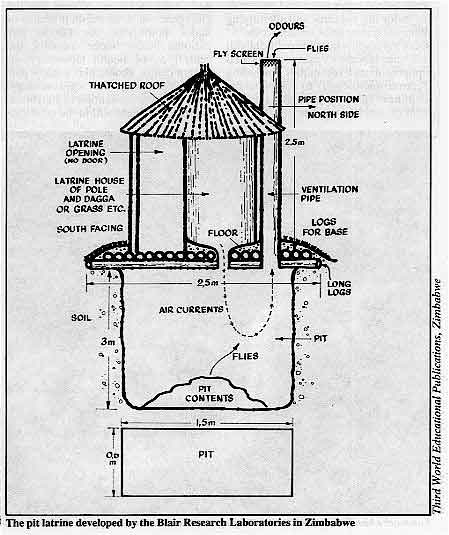
Zimbabwean latrines
Although pit latrine technology is basically simple, the effectiveness and
acceptability of the designs that have been developed varies enormously.
|
The pit latrine developed by the Blair Research Laboratories in
Zimbabwe
One successful latrine has been produced in Zimbabwe by the Blair Research
Laboratories. The super-structure is a doorless spiral with a large external vent pipe
(see illustration). Lack of a door means that the latrine can always be kept dark - very
important for fly control. Any flies that do manage to get into the pit escape via the
external vent pipe. Ventilation is improved by the vent pipe and the absence of a cover
(which can itself become contaminated) for the squat-hole.
More than 30,000 of these latrines have been built and are estimated to be in use in
Zimbabwe. A superior permanent structure is available in kit form for around $100.00, but
the same design can also be built from mud and wattle or other local materials for around
$7.00. The building instructions issued by Blair Research Laboratories strongly emphasize
how the system works to avoid mistakes in construction. If the latrine is built properly,
and therefore works well, the likelihood of its being accepted and used is much greater.
|
 |
For further information about the Zimbabwean latrine, write to Richard Middleton,
Technical Advisory Group, World Bank, 1818 H Street, Washington DC 20433, USA.
| In the next issue... In 1883, research into cholera was made
possible through Koch's discovery in Egypt of the comma bacillus or vibrio. Our first
issue in 1983, Diarrhoea Dialogue 12, will review the
achievements in cholera control over the past century. We will also look at parasitic
diarrhoea. |
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  3 Page 4 5 3 Page 4 5
| Laboratories and diarrhoeal disease control |
Collection, transport and examination
Laboratory services must work at all levels to be effective. Katherine
Elliott and William Cutting consider some ways in
which this can be achieved. Laboratory services of varying complexity play their part in the investigation of
diarrhoea at:
- primary health care centre level (especially useful in rural areas) using simple
equipment to examine specimens and to prepare them for transport.
- intermediate referral level, usually at a district hospital's clinical laboratory with
special equipment and materials for culturing bacteria and identifying them using a range
of suitable tests.
- central level, where the public health reference laboratory uses sophisticated equipment
and techniques (including electron microscopy) to complete the identification of the
pathogen referred from clinical laboratories.
The value of an integrated approach
Most countries with diarrhoeal disease programmes will, in addition to their clinical
laboratories, require a public health reference laboratory to investigate outbreaks of
infectious diarrhoeal diseases, to assist with control and preventive measures, to
supervise the testing of water supplies and to monitor and warn medical officers of the
emergence of drug-resistant strains of major pathogens. As far as any national health
budget permits, the central public health laboratory, or similar centre, should play a
major part in investigating the epidemiology, treatment and prevention of
diarrhoea-causing pathogens within the country. If the problem of diarrhoeal disease control is approached in an integrated way from
the outset, this will facilitate the most effective use of all available resources. This
should include primary health care workers in remote, rural areas whose role -
particularly in health education and the proper use of oral rehydration therapy - is
crucial. Good communication is essential between all levels of any country's laboratory
service to achieve and maintain reliability. Interchange of staff promotes better
understanding of local constraints and helps to integrate the service as an effective
whole. Handling specimens
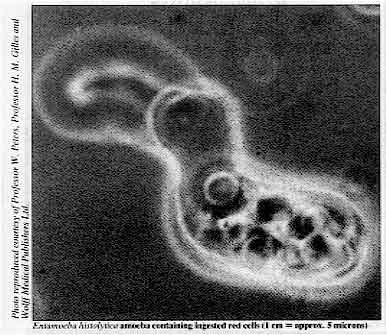 |
Entamoeba
histolytica amoeba containing ingested red cells. Health workers should know when and how to collect stool samples and how to send them
quickly and safely to the nearest laboratory. The history of illness must be recorded
accurately. indicating the presence or absence of fever. whether the problem is acute or
chronic, and notes should be made about the appearance and volume of the freshly passed
stool. It is possible to distinguish between dysentery (invasive diarrhoea with blood and
pus in a small, soft or loose stool) and secretory diarrhoea which produces a very large
liquid and watery stool.
|
At the health centre, simple equipment permits differentiation of bacillary dysentery,
most often shigellosis. from dysentery due to parasites, especially Entamoeba
histolytica. The="#page6">practical advice page in this issue gives
details of how to investigate diarrhoea at this level. The time taken in transport is important. Specimens of faeces should reach the referral
laboratory within two hours or otherwise be specially prepared for longer transport (see="#Transport">box). A health centre can prepare specimens in this way for
transport if supplied with the necessary instructions and materials. The preparation of
the appropriate media requires special facilities, including access to an autoclave and
this process is normally undertaken at referral laboratories.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  4 Page 5 6 4 Page 5 6
| Laboratories and diarrhoeal disease control |
Laboratory technicians
 |
Laboratory technicians play a very important role.
The technician in any laboratory has a very responsible role. The results of tests play
an important part in making decisions about treatment. Care, reliability and accuracy are
essential. (Better to admit to a mistake in the laboratory than to run the risk of a mistake in
treating the patient). Sound training is required and should be based on local health
needs and the facilities that are likely to be available.
|
Safety must never be neglected in any laboratory, however simple. Equipment must be
correctly installed and maintained. Specimens often contain highly infectious organisms
and their safe disposal is of utmost importance. Laboratory workers must practise a high
standard of personal hygiene which includes the washing of hands after handling specimens.
Protective clothing should be worn and left in the laboratory. Reagents and chemicals must
not be mouth-pipetted and any eating, drinking or smoking in the laboratory should
be forbidden. New techniques
The new API Z simple screening test of non-lactose fermenting colonies for salmonella
and shigella is enzyme-based, commercially produced, gives a result after only two hours
incubation and is relatively inexpensive. A variety of new rotavirus screening tests for
field use are now available as part of the ELISA range. The BIKEN Institute in Japan has
developed a simplified test to identify enterotoxigenic E. Coli (ETEC). If you
would like more details about any of these tests, write to Diarrhoea Dialogue.
|
Collection
Specimens should be collected as soon as possible after the diarrhoea begins and before
any antibiotics are given. A clean, dry and disinfectant-free receptacle must be used to
collect the faeces. Contamination with urine should be avoided. The next step is to use a
spoon, or wooden spatula, to transfer a portion of the stool, especially any part of it
that contains blood or mucus, into a clean, dry, (need not be sterile) leak-proof
container. Waxed paper cartons with lids, if available, are convenient but any leakproof
small container will do. A piece of faeces about 15-20mm in diameter is enough - or, if
the stool is liquid, about 5ml (in either case, a good teaspoonful). If worms, or segments
of tape-worms can be seen, these should, if possible be placed in a separate
container. Containers must be clearly labelled and be accompanied by a properly completed
request form. The presence of blood, mucus, worms and tape-worm segments should be noted. Where it is not possible to obtain a sample easily, for example from a baby, a
specimen can be collected by inserting a cotton or alginate wool swab into the rectum for
about ten seconds. Do not use lubricating gels. Make sure that the swab is well stained
with faeces. An alternative method is to insert a finger covered with a plastic fingerstall instead
of a swab. Care should be taken to avoid unnecessary contamination of the specimen with
bacteria from the skin surrounding the anus. The swab or fingerstall should then be placed
in a container as above, breaking off the swab stick to fit.
|
Transport
If delay in transport to the appropriate laboratory cannot be avoided, two or more
swabs from the stool should be inserted into a bijou bottle containing a suitable, sterile
transport medium such as Stuart or Cary-Blair, breaking off the swab sticks to allow the
bottle top to be tightly replaced. Cary-Blair medium preserves all enteric bacterial
pathogens and prevents them from being overgrown by the normal bacteria always present in
the bowel which do not cause diarrhoea. The media should always be inspected before use.
If already cloudy, they are probably contaminated and useless. Try a different bijou
bottle. Pathogens survive better in transport media if they can be kept as cool as
possible and in the dark. Salmonella, shigella, vibrio and yersinia organisms all survive well in Cary-Blair
medium at ambient (normal surroundings) temperature for up to two days. Campylobacter
survives for up to six hours only. If the specimen is for the culture of salmonella and
shigella organisms only, buffered glycerol saline can be used as transport medium. If
cholera is suspected, about 2ml of the fluid specimen should be placed into a container of
sterile, alkaline peptone water which encourages the growth of vibrio organisms. If
amoebic dysentery or other parasite infection seems likely and it is not possible to
examine a fresh faecal specimen as described on="#page6">page six, a small
amount (0.5gm) of the stool should be transferred into a bijou bottle containing freshly
prepared merthiolate iodine formaldehyde (MIF) fixative. This fixes protozoal parasites
for later examination. Bacteria are also killed in MIF and faeces preserved in this medium
cannot be cultured. Where rotavirus is suspected about 1g of faeces (preferably from a stool rather than a
swab) may be stored in phosphate buffered saline for analysis by the ELISA method. Label clearly and pack properly in all instances, including always the matching,
completed request forms preferably in a polythene bag. Remember the bijou bottle contains
live organisms! Great care should be taken to clean and disinfect everything that comes
into contact with stool specimens from patients with diarrhoea. Faeces can be very
dangerous and should be handled accordingly.
|
|
We would like to thank Bernard Rowe, Director, Central Public Health
Laboratory, London; Peter Humphries, Principal MLSO at the Royal Free Hospital, London and
Monica Cheesbrough, author of a Medical Laboratory Laboratory Manual for Tropical
Countries for their advice and comments on this article.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  5 Page 6 7 5 Page 6 7
Simple laboratory investigations into
diarrhoea
Tony Moody looks at the range of laboratory work that
can be carried out at health centre level. The complete investigation of diarrhoea requires complex and sophisticated laboratory
techniques to isolate and characterize the causative agent. This does not exclude the
laboratory worker with only simple, basic equipment from being able to provide useful
information for the management of diarrhoea.
Essential laboratory equipment consists of:-
- a microscope
- microscope slides and coverslips
- saline solution
- pipettes
- some basic stains and litmus paper
Total cost - less than $500 US dollars. Macroscopic appearance
Useful information can be gained by careful inspection of the faeces with the naked eye
(1). The history of the patient's diarrhoea should be kept in mind whilst looking at the
faeces. The Clinician's Guide to Aetiology published in="dd07.htm">Diarrhoea
Dialogue 7 and the new wall charts now available from the Ross Institute
of Tropical Hygiene* may be useful aids in this preliminary screening.
- Profuse watery stools, sometimes flecked with mucus, occur in toxigenic E. coli diarrhoea
and in cholera (rice water stool).
- Smaller, soft and frequent stools containing blood and mucus occur in amoebic dysentery
and in bacillary dysentery due to shigella or campylobacter infections.
- Pale, frothy stools occur in giardiasis, tropical malabsorption and in lactase
deficiency in infants.
Acid or alkaline reaction (pH) A simple litmus paper check on the stool pH can
be helpful. Acid stools occur in amoebic dysentery and in lactase deficiency. In bacillary
dysentery the stool is alkaline. Microscopic examination
The stool should be as fresh and warm as possible when examined. Saline preparation
Place a drop of saline (0.9% sodium chloride) at room temperature onto a warm slide and,
selecting an appropriate section of the faeces, i.e. from an area of bloody mucus or from
the liquid part of the sample, use a stick to transfer a small amount to the slide.
Emulsify this in the saline and place a coverslip over the preparation (discard the stick
safely into disinfectant or burn). Examine the sample under the microscope using a 10x
eyepiece and, initially, a 10x objective. Close the condenser iris diaphragm sufficiently
to give good contrast. Careful searching of the whole coverslip area at this magnification
could reveal active larvae of Strongyloides, ova of Schistosoma or other
helminths, or clumps of pus cells and erythrocytes which indicate an inflammatory response
to bacteria or amoebae. Now turn the 40x objective into the viewing position and again search the whole
coverslip area. Dysentery
At this level of investigation, the most important distinction that can be made is between
amoebic and bacillary dysentery. Both stools may contain pus cells and macrophages and
these show up well if a drop of 1% methylene blue stain is run under the coverslip. There
may also be erythrocytes (red blood cells) in the stools. In amoebic dysentery, if the specimen is fresh (still warm), very active trophozoites
of Entamoeba histolytica (20-40 microns in size, i.e. about twice the size of
polymorph leucocytes (pus cells)) ought to be easily observed moving rapidly across the
slide, pushing out clear pseudopodia and containing ingested red blood cells. There should
be no confusion between amoebae and macrophages which may also contain red blood cells.
The amoebae move about and constantly change shape. The macrophages become immobile within
a few seconds. In bacillary dysentery, caused by infections such as Shigella,
Campylobacter and possibly invasive E. coli, there will be many pus cells,
erythrocytes and macrophages, but no active amoebae or cysts. (Occasionally patients may
have both amoebic and bacillary dysentery at the same time). Flagellates
Few or no cells in a fatty or unformed sample may indicate the cystic or trophozoite
stages of Giardia lamblia in the saline preparation. The refractive axostyle and
flagellar components of the cysts can be shown more clearly by using an iodine stain (1 in
5 dilution of Lugol's iodine in 10% acetic acid). A thin saline suspension of faeces
smeared on a slide, air dried and fixed in methyl alcohol can be stained with a 1 in 20
dilution of Giemsa stain in pH 6.8 buffer for 15 minutes and will demonstrate the
morphology of the trophozoites of Giardia. Fat is seen as yellow globules or fine
needles and can be stained red with 1% alcoholic Sudan 111 stain. Other flagellates may be present but are not pathogenic. Vibrio cholerae
Dark ground illumination and a hanging drop preparation are needed to identify the
darting motility associated with cholera vibrios. A dark field condenser costs about £90
to modify a normal microscope. A temporary version can be contrived using plasticine or
putty to use with the 40x objective (see page 61 in volume 1 of Monica Cheesbrough's Medical
Laboratory Manual for Tropical Countries - reviewed on="#page7">page
seven). Hanging drop preparation
Take a slide and make a ring of about 1cm using Vaseline. Place a coverslip flat on a
table, add one drop of the liquid stool in the centre and place the Vaseline ring on the
slide over this drop. Quickly invert the slide and inspect under the 40x objective for the
typical darting movement by rod-shaped organisms. Tony Moody, Senior Chief MLSO, Hospital for Tropical Diseases, St Pancras Way,
London NW1, U.K. (1) Banu et al 1982 Epidemiologic and clinical features of patients infected with
shigella who attended a diarrhoeal diseases hospital in Bangladesh. The Journal of
Infectious Diseases, Vol. 146 no 2: 177-183.
*Inquiries to Dr Isabelle de Zoysa, Ross Institute of Tropical Hygiene, London
School of Hygiene and Tropical Medicine, Keppel St, London WC1, U.K.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  6 Page 7 8 6 Page 7 8
Books for medical laboratory workers
Peter Humphries reviews three laboratory manuals that
include investigation techniques for diarrhoea. A Medical Laboratory Manual for Tropical Countries
(Volume 1, first edition 1981. Volume 2 in preparation - due for
publication in June 1983)
Monica Cheesbrough (author and publisher)
Price: £4.70 (developing countries) * £7.60 (other countries) * The author has kindly provided pre-publication text for review from the microbiology
section of Volume 2. Volume 1 contains the parasitology of stools and fully describes the helminths and
protozoa causing diarrhoea. Methods are carefully and singly explained, well illustrated
with detailed notes on likely problems. The author's personal experience of most of the
techniques given is clearly demonstrated. The text is up-to-date and presented in a
friendly style. Safety procedures are a welcome inclusion, too often omitted from
descriptive manuals. In addition to its full technical repertoire the text includes
introductory material and explains the clinical relevance of the laboratory procedures
described. The microbiology section previewed from Volume 2 includes a definitive investigation of
diarrhoea as a clinical entity. Modern ideas about tropical diarrhoea are fully explained
together with associated laboratory procedures which include instructions for workers at
all levels of health care. Technical matters are absolutely up-to-date and will prove
useful for the modern laboratory anywhere in the world. Again, the author has achieved a
friendly, communicative style without losing the authority which underlies all the
material in the section reviewed. Of the three manuals reviewed, these two volumes by Monica Cheesbrough can be
recommended for medical laboratory workers anywhere. Whatever facilities they have, there
will be something to improve their services to health care. *Postage and packing for developing countries is £1.25 and £1.75 elsewhere. You
can obtain the manual by writing to Monica Cheesbrough, 14 Bevills Close, Doddington,
Cambridgeshire PE15 0TT, UK. Visitors to London can obtain the manual from the Institute
of Child Health, 30 Guildford Street, London WC2.
Manual of Basic Techniques for a Health Laboratory 1980
(New edition in preparation)
World Health Organization
Price: 30 Swiss Francs (approximately £8.50)* This book is a mixture of reference material and illustrated techniques, both aspects
freely intermingled, a feature which is sometimes confusing. Diarrhoea is not treated as an entity and does not appear in the index, but it does
appear in various places when the condition is associated with the parasite under
discussion. The reference aspect is extremely detailed with useful size comparison charts for
helminth ova and pictures of artifacts. Style is strictly factual which can be expected in
a laboratory reference manual. Technical instructions are also described in an impersonal
style, leaving out much important detail, in contrast to the reference text. Sections on concentration methods are well illustrated and given for a variety of
infections including strongyloides larvae. Excellent instructions are given for despatch
of stools for parasites and bacterial cultures to laboratories where these investigations
can be carried out. There are some surprising omissions for such a recent text, particularly on clinical
links with the investigations described. This is a book for the laboratory shelf, rather
than a friendly companion. * You can obtain this manual by contacting your WHO regional office or writing
directly to WHO headquarters in Geneva. Postage will depend on where the book is being
sent. WHO, 1211 Geneva 27, Switzerland.
Medical Laboratory for Developing Countries 1972
(latest edition)
Maurice King
Oxford University Press
Price: £3.50* The word diarrhoea does not appear in the index, nor is the condition treated as an
entity. However, Chapter 10 deals fully with the examination of stools, concentrating on
macroscopic and microscopic methods for helminths and protozoa. The text is very detailed,
accompanied by easily followed diagrams and pictorial sequences of techniques. The
formaldehyde-ether method is the only concentration technique described and its
limitations are not fully explained. The coverage of diarrhoea is limited to bacillary and amoebic dysentery, giardiasis and
lactase deficiency in infants. The importance of macroscopic appearance of stools for
signs of helminths or exudates is emphasized and a method for estimating the pH of stools
is described. Stool culture for bacteria is omitted and no instructions are given for
stool transport to laboratories where this can be done. There are many tips for carrying out the procedures described with homemade tools and
the style of the text is simple and friendly. Nevertheless, conceptual and technical
advances in the investigation of tropical diarrhoea have overtaken some of the fundamental
ideas in this book, due mainly to the length of time since its publication. * Postage will depend on where the book is being sent. For details write to Oxford
University Press, 37 Dover Street, London W1, UK. Peter Humphries, Principal MLSO, Royal Free Hospital, Pond Street, London NW3, UK.
|
|
DDOnline
Diarrhoea Dialogue Online Issue 11 November
1982  7 Page 8 7 Page 8
ORT in Tamil Nadu
|
Health
workers being trained in Tamil Nadu
We very much appreciate oral rehydration therapy in diarrhoeal illnesses. This is the
first measure we have taken in primary health care along with our leprosy control work. We
advise the mothers to use a palade (a small metal vessel used for feeding
young babies) to measure sugar and common salt and an empty gripe water bottle to measure
out adequate water. Both the palade and the bottle are common household articles in Tamil
Nadu.
|
 |
These are the quantities we use to prepare the oral rehydration drink:
- one level palade full of sugar (7.0gm)
- one level palade spout-full of salt (1.0gm)
- one small pinch of baking soda
- dissolved in one gripe water bottle of clean water (130ml)
This drink is very palatable and well accepted by children. We are very happy to share
this information with you. Dr Mohan, Kasturba Nilayam, Malavanthangal, Via Kandachipuram, S. A. Dt. 605701,
T.N., India.
Village programmes
We have nine expert nurse midwives here and an auxiliary training programme with 15
students at present. Mass Media from the USA are distributing 200,000 pictures showing how
to make sugar-salt solution. In many villages the person who has been shown how to make up
the solution has a flag (a black baby on a pink background) so that people in the
compound know where to go for help. We find that, after instruction, mothers are giving
the sugar-salt solution, but sometimes continue it for longer than recommended before
getting further help. Instructions for making up the solution have also been given on Radio Gambia and there
is certainly a great deal of interest. Dr John E. Matthias, Banjul, The Gambia, West Africa.
Soya milk
I was surprised that no mention was made on="dd06.htm#page6">page six of Diarrhoea
Dialogue 6 (Persuading children with diarrhoea to eat) of soya beans. We find them
a real godsend, especially for making soya milk to give to children with diarrhoea. This
'milk' is high in protein content and lactose-free. It contains about three quarters of
the calcium supplied in breast milk and also has a satisfactory iron and Vitamin B
content. We cannot unreservedly recommend soya milk as the sole food for infants under four
months, who, in any case should be breastfed. However, it is extremely useful for
alternative or temporary feeding, or for infants with diarrhoea. We have included a recipe
for making soya milk so that other people can try it.
- Wash, sort and soak 500gm soya beans in plenty of clean water overnight.
- Mince or grind the beans.
- Boil two litres of water and add the minced beans. Bring back to the boil. Stir and be
careful the mixture does not boil over. Boil for 15 minutes.
- Strain through a clean cloth or wire sieve. Add a pinch of salt and some sugar to taste.
Anna Pearce, Compassion, Brooklyn, Capetown, South Africa.
Traditional remedy in India An article in="dd06.htm">DD 6 about the use of rice water and rice
porridge for rehydration reminded me of my grandmother's remedy, which saw three
generations of children safely through diarrhoea episodes, usually without any other
medication. This is a porridge of sago (known locally as saboodana or sabbiyam) cooked in
water to a gelatine-like consistency, served with salt and sugar to make it palatable.
Milk or buttermilk were added as soon as the condition improved, to take care of the need
for protein. 4-5 helpings were given, 8oz for adults and proportionately less for
children. Most children enjoy the bland flavour of this preparation, it is highly
effective and cheap. Ms Srilatha Batliwala, Bombay 400 018, India.
|
Scientific editors Dr Katherine Elliott and Dr William Cutting
Executive editor Denise Ayres Editorial advisory group
Professor David Candy (UK)
Dr I Dogramaci (Turkey)
Professor Richard Feachem (UK)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr D Mahalanabis (India)
Professor Leonardo Mata (Costa Rica)
Dr Mujibur Rahaman (Bangladesh)
Dr Jon Rohde (USA)
Ms E O Sullesta (Philippines)
Dr Paul Vesin (France)
Dr M K Were (Kenya) With support from WHO, UNDP, GTZ and SIDA
|
Issue no. 11 November 1982
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
|