|
| |
Issue no. 43 - December 1990
pdf
 version of this
Issue version of this
Issue
|
There is much information in this issue that is valuable
and useful. Online readers are reminded, however, that treatment guidelines and health
care practices change over time. If you are in doubt, please refer to
WHO's up-to-date Dehydration Treatment
Plans.
|
Pages 1-8 Dialogue on Diarrhoea Online Issue 43 -
December 1990
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  Page 1 2
Page 1 2
More about drugs and diarrhoea
No-one could wish to go back 50 years to the time before antibiotics were discovered,
when infections proved too often to be killers. Previously healthy children, given good
nursing with proper fluid and food intake, usually survived because their own natural
resistance was stronger than that of the invading bacteria. Weaker and deprived children, however, too often died - or suffered permanent damage to
health and growth. Penicillin, and all the other antibiotics which followed, dramatically
improved the chances of growing up healthy. But, as DD42 explained,
all powerful drugs must be correctly used and not abused, if they are to remain effective.
The theme continues in this issue. More harm than good
Diarrhoea can be frightening and mothers understandably want to stop it. In 1982, DD8 advised readers against dangerous preparations which
claimed to 'turn off the tap' in diarrhoea. No such safe drug as yet exists. Drugs that
reduce the stool output by slowing down or paralysing the gut (antimotility drugs - see="#page4">pages 4 and 5) should never be given to
young children. They make children sleepy. It is then more difficult for them to take
sufficient food or fluid. Dangerous dehydration becomes an even greater threat and full
final recovery more difficult to achieve. There can also be severe side effects.
|
Parents often ask for medicine for a child with
diarrhoea, but most 'anti-diarrhoeals' are unsafe for young children; ORT is always the
best treatment. The safest and the most effective treatment for acute diarrhoea is still to give enough
fluid to replace the water and salts lost in stools. If rehydration begins at once,
appropriate fluids can usually be given by mouth.
|
 |
Intravenous drips and nasogastric tubes are needed only in very severe or neglected
cases where there is circulatory collapse, excessive vomiting or unconsciousness. The need
to prescribe drugs may have to be considered later, depending on the probable cause of the
diarrhoea. However, the growing problem of antibiotic resistance calls for a much more
cautious approach to antibiotic use by all health professionals and also by the public
(see="dd42.htm">DD42). Prevention as well as cure
Because good medicine should always be concerned with prevention, this issue of the Dialogue
includes ways to promote low cost sanitation (page 7), the
treatment of worm infestation (page 6), and emphasises the invaluable
protection offered by breastfeeding (page 2).
|
In this issue:
- Antimotility drugs reviewed
- Changing prescribing practices of doctors in Mexico
- Low cost sanitation in Lesotho
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  1 Page 2 3 1 Page 2 3
Abstracts Antibiotic resistance
This study compared resistance of faecal E. coli from healthy children
(i.e. not patients currently receiving treatment) to antimicrobial agents in three cities
in the USA, Venezuela and China. Much higher levels of resistance were found in Venezuela
and China - all but one of 41 children in Caracas, and all but two of 53 in Qin Pu carried
resistant strains - whereas 18 of 39 children in Boston had no resistant colonies. Only
one child in Boston, but 25 in Caracas and 34 in Qin Pu carried strains resistant to
trimethroprim; and 17 children in Qin Pu also carried strains resistant to
gentamicin. The
study shows that resistance of bacteria in healthy children varies greatly from region to
region, probably reflecting more frequent use of antibiotics where resistance is most
prevalent. Since infections with resistant bacteria are difficult to treat, efforts are
needed to reduce the frequency of resistance by using antibiotics more selectively,
i. e.
only for infections where their benefit is proven. Lester, S C, et al., 1990. The carriage of E. coli resistant to antimicrobial
agents by healthy children in Boston, in Caracas, Venezuela and in Qin Pu, China. New Eng.
J. Med. 5 (323): 285-9. Breastfeeding prevents infection
1. Over 600 pairs of mothers and infants in the UK were
studied to assess the links between breastfeeding and illness in the first two years of
life, with special reference to diarrhoeal disease. Health visitors observed infant
feeding practices and infant illness at two weeks of age, monthly for six months and then
at three monthly intervals.
 |
Increasing scientific evidence shows that breastfeeding is best.
Babies who were breastfed for more than three months had significantly less diarrhoea
than those bottle-fed from birth. This reduction in illness was found whether or not
supplementary foods were given before three months of age. Babies breastfed for less than
three months had similar rates of diarrhoeal illness to bottle-fed babies. Babies
breastfed for more than three months had less diarrhoea for all of the two years of the
study than bottle-fed babies, and fewer needed admission to hospital.
|
Breastfeeding during the first three months of life gives protection against diarrhoeal
disease; the protective effect appears to continue after breastfeeding is stopped. Howie, P W, et al., 1990. Protective effect of breastfeeding against infection.
Brit. Med. J. 300 (6 January): 11 -16. 2. We studied the effect of breastfeeding in preventing
diarrhoea caused by Campylobacter jejuni in 98 Mexican children for two years from
birth. Total diarrhoea incidence was 2.3 times less in breastfed children under six months
old than in bottle-fed children of the same age. Breastfed children also remained free of
diarrhoea for longer than bottle-fed children. Campylobacter diarrhoea occurred less often
in the breastfed group than in the bottle-fed group. Our investigation showed that special
antibodies which protect against Campylobacter and other diarrhoeal infections were
transferred from mother to baby in breastmilk. Breastfeeding is therefore an important
protection for babies against diarrhoea. Ruiz-Palacios, G M, et al., 1990. Protection of breast-fed infants against
Campylobacter diarrhea by antibodies in human milk. J. Ped. 116( 5): 707-13. Comment: Several studies from developing countries have shown that protection against diarrhoea
declines when other foods or fluids are given as well as breastmilk, and disappears when
breastfeeding is stopped. Infants are especially vulnerable to diarrhoea when weaning
foods are introduced, as these may be contaminated. It is therefore especially important
that breastfeeding is continued after three months and when other foods and fluids are
given. ORS better than drugs
In India, packets of ORS are to be promoted and made widely available to families by
all health workers and pharmacists. In the past, health workers were encouraged to give
ORS packets for cases of severe dehydration, and to recommend home fluids for mild cases.
This decision follows an extensive nationwide study of mothers and practitioners in rural
areas.(1). The study found that the unnecessary use of anti=diarrhoeals and antibiotics is
greatest in mild cases. Because many mothers insist on having some form of 'medicine',
even for mild diarrhoea, it is better to give them ORS than potentially dangerous drugs.
For this reason, the Indian Ministry of Health and Family Welfare has decided to make ORS
packets much more widely available. 1. Diarrhoea in Rural India: for information contact UNICEF, 73 Lodi Estate, New
Delhi 110003, India. Folate for diarrhoea?
We carried out a controlled clinical study of 76 infants and young children admitted to
hospital with acute diarrhoea. Patients receiving an oral dose (5mg every 8 hours) of
folate (also called folic acid, a vitamin of the B complex) recovered in a significantly
shorter time (mean 53 hours) than those not given folate (mean 92 hours). All received
ORT, while intravenous fluids were given only to those with severe dehydration and shock,
or with repeated vomiting. Breastfeeding and/or formula feeding were continued from the
time of admission. (In three folate patients and in nine controls, cow's milk formula had
to be replaced by a soya feed after three days due to continuing diarrhoea). There were no
adverse side effects of the folate. We chose to use folate because its importance in cellular DNA synthesis may accelerate
the normal regeneration of damaged villous cells of the small bowel. This is how it may
help in rotaviral diarrhoea, which damages the villous tips. But there were equally good
results in patients with non-rotaviral diarrhoea, so this cannot be the only explanation.
No infants in the same population had shown any evidence of folate deficiency in an
earlier pilot study. Although further trials with larger numbers of patients are needed, it appears that
this non-allergenic, cheap and readily available therapy could play an important role in
shortening the duration of childhood diarrhoea and possibly in preventing or modifying
persistent diarrhoea. I E Haffejee, Department of Paediatrics and Child Health, University of Natal,
PO Box 17039, Congella 4013, South Africa. Haffejee, I E, 1988. Effect of oral folate on duration of acute infantile
diarrhoea, Lancet ii: 334-5.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  2 Page 3 4 2 Page 3 4
Physicians' behaviour
A project in Mexico City has succeeded in changing the way doctors prescribe for
diarrhoea. Oral rehydration therapy (ORT) is the recognised safe and effective treatment for acute
diarrhoea. In some cases, such as shigellosis, antibiotic treatment is also recommended.
Antibiotics are, however, given far too often, and the misuse of drugs is a leading cause
of antibiotic resistance (see="dd42.htm">DD42). Usage patterns are
influenced by the prescribing practices of physicians, pharmacists and others who sell
drugs. ADDR has funded studies to identify such practices and to develop interventions to
change them. Dr Gutierrez and colleagues(1) at the Mexican Institute of Social Security
(IMSS)
studied the prescribing practices of physicians for patients with acute diarrhoea. The
study also looked at ways to promote ORT use for all patients under five, to limit
antibiotic use to cases where it is indicated (about 10 per cent of diarrhoea patients),
and to avoid restricted diets and anti-diarrhoeal agents, both of which may be harmful. Collecting baseline data The prescribing practices of 69 physicians (including 20 controls) were observed for
401 randomly selected children with acute diarrhoea seen at two clinics in Mexico City.
The twenty physicians who served as controls did not attend education sessions but had
copies of the recommended treatment scheme. Antibiotics were prescribed for 76 per cent of
cases and ORT was prescribed for only 34 per cent. Other drugs (kaolin-pectate,
antipyretics, antiemetics), as well as restricted diets, were also often prescribed. After baseline data collection, participating physicians attended a workshop where they
learned about the study, discussed the findings and recent literature on acute diarrhoea,
and designed a therapeutic scheme based on clinical data. The scheme recommends treatment
in Mexico as listed below.
- All children under five with acute diarrhoea should have ORT plus continued feeding with
a non-restricted diet.
- Antibiotics should not be given unless bloody diarrhoea is present.
- Patients with bloody diarrhoea but without fever and/or toxicity probably have
amoebiasis and should receive metronidazole.*
- Patients with bloody diarrhoea plus toxicity probably have shigellosis and should
receive ampicillin or trimethoprim - sulfamethoxazole.
Following the training session, the prescribing practices of all the available workshop
participants (36) treating 202 cases of acute diarrhoea were recorded for four months. At
the end of this period, a second educational session was begun. In this new intervention,
their prescribing practices were evaluated and discussed with a peer committee composed of
a researcher, a senior physician, and three study physicians. After the peer review, the
prescribing behaviour of participants and controls was again assessed. Measuring behaviour change The study found that the workshop and peer review committee produced sustained changes
in prescribing behaviour. Prescription of antibiotics or anti-parasitic drugs by the
participating physicians fell from 78 per cent of cases at baseline to 38 per cent of
cases six months after the intervention. At 18 months after the intervention, this rate
had increased slightly to 43 per cent.
|
A Mexican
doctor explains how to use ORT. ORT use rose from 35 per cent at baseline to 68 per cent at six months and 62 per cent
at 18 months. Prescription of non-restricted diets rose from 54 per cent to 90 per cent
after six months and 9 1 per cent at 18 months. In contrast, the prescribing behaviour of
control physicians was unchanged.
|
 |
Dr Gutierrez points out that major savings in costs, resulting from reduced use of
drugs, were an additional benefit of the educational intervention. A second grant from ADDR will enable the IMSS group to test their intervention at 18
clinics. If this second study is successful, the group hopes to implement the intervention
in a Mexican state. Dr Gonzalo Gutierrez, Hortensia #57, CoI Florida, 01030 Mexico DF, Mexico. 1. Guiscafre, H, et al, 1988. Evaluation of the strategy designed to promote
changes in the prescription pattern of oral hydration, antibiotics and restrictive diet by
family physicians. Arch. Invest. Med. 19: 395-407. This paper is one of ten articles in a special issue of Archivos de Investigacion
Medica (Vol 19, No 4, October-December 1988) devoted to proper use of medications for
therapy of diarrhoea. * WHO/CDD note: Amoebiasis is rare in children less than five years of age, and
shigellosis can cause bloody diarrhoea without fever. CDD does not advise metronidazole as
initial treatment for bloody diarrhoea, but only when treatment for Shigella has failed or
E. histolytica trophozoites are seen in the stool.
The ADDR Project For five years, since 1985, the Applied Diarrheal Disease Research
(ADDR) Project has
provided grants and technical assistance to approximately 175 researchers in developing
countries who are studying various aspects of diarrhoeal diseases. The Project, funded by
USAID, is implemented through the Harvard Institute for International Development;
collaborating institutions are the New England Medical Center and Johns Hopkins
University. ADDR has been extended for two more years to enable researchers to analyse and
report results from 85 ongoing studies. ADDR supports research in four areas:
- home use of food and fluids in the management of diarrhoea
- prevention and intervention studies
- invasive and persistent diarrhoea
- behaviours of mothers, care-givers and health care providers.
Most projects have been located in seven countries: Peru, Mexico, Nigeria, Kenya,
Pakistan, Thailand and Indonesia. Selected results will be published in Dialogue on
Diarrhoea; the first of these appears in this issue. Enquiries should be sent to: ADDR
Project, Harvard Institute for International Development, 1 Eliot Street, Cambridge, MA
02138, USA.
|
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  3 Page 4 5 3 Page 4 5
Antimotility drugs
'Anti-diarrhoeal' drugs should not be used for the treatment of acute diarrhoea in
children. This issue of DD previews information, soon to be published by WHO, on two
widely used antimotility drugs. Loperamide
There is no evidence that loperamide reduces fluid and electrolyte losses in
children with acute diarrhoea. Its antimotility effects may make bacillary dysentery
worse. In children aged under six months it depresses the central nervous system. For
these reasons, loperamide should not he used in the management of childhood diarrhoea.
There is no rationale for its production and sale in liquid and syrup forms. Formulation
A man-made opium-like drug developed specifically for use in diarrhoea. Available in
tablet, liquid and syrup forms under a variety of brand names. Pharmacology Poorly absorbed. Ten per cent of the dose given is recovered in the urine, and about 40
per cent is excreted unchanged in the faeces. How it works
Loperamide inhibits propulsive (peristaltic) movement in the small intestine by
affecting the intestinal smooth muscle.(1) It also affects intestinal motility by
inhibiting prostaglandin stimulation of gut motility, and directly or indirectly
depressing the bowel stimulation by calcium. (2) Loperamide has not been shown to increase
fluid absorption in the gut. There is little firm evidence that it decreases intestinal
fluid secretion especially at the recommended doses.(3) Efficacy Most studies assessing the efficacy of anti-diarrhoeals have measured stool fluid loss
or bowel movement, or both. Many were poorly designed and the results were therefore
unclear. Loperamide has been shown to reduce stool output in some children with some forms
of chronic diarrhoea in developed countries, by an average of less than one stool per day,
but only with doses at least twice as high as those conventionally given. The same effects
have not been seen in children with persistent diarrhoea in developing countries. Clinical
trials in children with acute diarrhoea, using the standard recommended dose and double
dosages, have not shown any effect on stool output. Some larger studies suggest that
loperamide may shorten the duration of diarrhoea by up to 24 hours, but only when using
two or four times more than the recommended dosage. (The standard recommended dose is
0.2mg/kg/day.(4) ) Adverse effects Adults with acute diarrhoea taking loperamide have occasionally reported side effects
including nausea, vomiting, drowsiness, dizziness, depression, blurred vision, abdominal
pain and headache. Occurrence of these symptoms in children has not been studied, but
adverse effects of loperamide on the CNS and gastrointestinal motility among infants and
young children are reported below. Central nervous system (CNS) effects Loperamide has CNS effects, especially in children aged less than six months.
Drowsiness has been seen in controlled clinical trials at dosages of 0.8mg/kg/day; CNS
depression at dosages as low as 0.1mg/kg/day; coma after doses of 0.5mg/kg/day and after a
single dose of 0.125mg/kg. In a study of 151 infants seen for drug poisoning in Mexico,
ten cases were related to loperamide; only two of these had exceeded (by more than
twofold) the manufacturer's recommended dose; six required treatment with opiate
antagonists. Gastrointestinal motility Abdominal distension and potentially fatal bowel paralysis have been reported in
infants and young children treated with loperamide. As a result, the drug's leading
manufacturer has halted the sale of loperamide drops and restricted the sale of loperamide
syrup in developing countries.( 5,6) Antimotility drugs such as loperamide can prolong the time that pathogens are found in
the stool. Antimotility agents have enhanced the pathogenicity of Shigella in animal
experiments. They have also prolonged fever and decreased clearance of pathogens in adults
experimentally infected with Shigella. 1. Kachel, G. et al., 1986. Human intestinal motor activity and transport: effects
of a synthetic opiate. Gastr. 90: 85.
2. Reynolds, l J, et al., 1984. Loperamide: blockage of calcium channels as a
mechanism for anti-diarrhoeal effects. J. Pharm. E. tp. Ther. 231: 628.
3. Schiller, L R, et al., 1984. Mechanism of the anti-diarrhoeal effect of
loperamide. Gastr. 86: 1475.
4. Diarrhoeal Diseases Study Group, 1984. Loperamide in acute diarrhoea in
childhood. Brit. Med. J. 289: 1263-7.
5. Bhutta, T I, and Tahir, K I, 1990. Loperamide poisoning in children. Lancet 335:
363.
6. Gussin, R, 1990. Withdrawal of loperamide drops. Lancet 335: 1603.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  4 Page 5 6 4 Page 5 6
Diphenoxylate hydrochloride
Diphenoxylate may help relieve symptoms of mild chronic diarrhoea in adults,
but there is no evidence of a beneficial effect in the treatment of acute diarrhoea. It
does not reduce fluid losses associated with diarrhoea and may interfere with fluid
replacement. It should not be used for children as it can have serious effects on the
nervous system at standard recommended doses. It may also worsen bacillary dysentery. It
is not recommended for the management of diarrhoea in children, and consequently there is
no reason for its production or sale in liquid or syrup form. Formulation
Diphenoxylate is also a synthetic opiate (related to pethidine and morphine) developed
for use in diarrhoea. It is sold in combination with a small amount of atropine to
discourage deliberate abuse of the drug. Typical formulations for oral medication contain
2.5mg of diphenoxylate and 0.025mg of atropine per tablet or 5ml of liquid. Diphenoxylate
is sold under a variety of trade names (Lomotil is one of the most common) and also in
combination with antibiotics. Pharmacology
Diphenoxylate is converted in the liver to a biologically active form which is excreted
mainly in the urine and bile. Its main time of action is probably two to five hours after
a dose has been given by mouth. How it works
Studies have shown that diphenoxylate reduces the rate of peristalsis - muscular
movement in the gut - and the flow of contents of the small intestine. It has been
suggested that the delay in faecal emptying allows more time for fluid absorption,
therefore decreasing fluid losses in the stool, but there is little evidence to support
this. Many studies have investigated the direct effects of opiate drugs on intestinal fluid
absorption and secretion. Morphine and some synthetic opiates decrease intestinal
secretion which has been stimulated by substances including prostaglandins and cholera
toxin. But there is no evidence to show that diphenoxylate has an antisecretory role or
that it promotes intestinal fluid absorption. Efficacy
In adults
Most early efficacy studies were carried out in adults with chronic diarrhoea. These
studies, though largely uncontrolled, suggested that diphenoxylate could decrease stool
frequency in patients with irritable colon and ulcerative colitis. In the late 1960s, to clarify the role of diphenoxylate in the management of acute
diarrhoea, the General Practitioner Research Group in England conducted two double-blind
trials with diphenoxylate. Neither trial showed that diphenoxylate therapy gave any
significant benefit in acute diarrhoea. In another double-blind trial in adults with acute
diarrhoea, a single 5mg dose of diphenoxylate had no effect on stool consistency. Diphenoxylate has been shown to be significantly less effective than tetracycline in
the treatment of cholera, and does not increase effectiveness if added to tetracycline
therapy. In children Various trials have assessed the efficacy of diphenoxylate therapy in children. But
most studies were poorly planned and gave doubtful results. In the only study to look at
whether measured stool fluid and electrolyte losses were reduced, diphenoxylate was not
effective. (1) In addition, neither this nor another blind trial showed a significant
reduction of stool frequency. (2)
The only double-blind trial to show any effect of diphenoxylate in children with
diarrhoea was a small study where the period of hospitalisation of malnourished infants
with acute diarrhoea treated with diphenoxylate was shorter, but no benefit was found in
children with chronic diarrhoea.( 3) However, the discharge criteria were not clear.
In another, larger double-blind trial in which the discharge criteria were more clearly
stated, diphenoxylate had no effect on the duration of hospitalisation. (2) Adverse effects Reported side effects from diphenoxylate therapy include anorexia, nausea and vomiting,
swelling of the gums, abdominal distension, paralytic ileus (bowel paralysis), toxic
megacolon (bowel enlargement), headache, drowsiness, depression, confusion, insomnia,
dizziness, restlessness, euphoria and skin reactions. In addition, the atropine content
may be associated with high fever, rapid pulse, urinary retention, flushing, and dryness
of the mouth. Central nervous system effects These are the most serious side effects and have resulted in coma and death. One study
of children, most under one year of age, observed drowsiness in 17 per cent of the
diphenoxylate-treated infants compared with 6 per cent of controls. Other similar rates of
sedation in children have been reported. (Drowsy children are less able to drink and
therefore harder to rehydrate.)
 |
Antimotility drugs make children sleepy, which stops them from
drinking.
Several cases of severe central nervous system toxicity with normal therapeutic doses
have been reported. In addition, dangerous overdose is common when repeated doses are
taken for severe diarrhoea cases, partly because diarrhoea does not stop quickly so
excessive doses are often given by mistake, resulting in coma or even death. Diphenoxylate
is also a common cause of accidental poisoning in toddlers.
|
Gastrointestinal side effects Abdominal distension has been reported in seven to 12 per cent of infants receiving
diphenoxylate therapy, but also occurs in untreated children with acute diarrhoea. Other
problems related to the slowing of gastrointestinal movement caused by antimotility drugs
include:
- delay in the clearance of pathogens from the stool. In Shigella infections in
experimental animals, opiates have actually been shown to increase penetration of the
infecting organism. Similar results were demonstrated in 25 volunteers given Shigella
germs in an experiment. The diphenoxylate also prolonged fever and reduced antibiotic
efficacy.
- retention of water and electrolytes in distended loops of the bowel. This could disguise
actual fluid losses and cause delay in seeking appropriate care and accurate fluid
replacement.
Definitions MOVEMENT or MOTILITY of the contents of the bowel is due to muscle movements called
PERISTALSIS. PERISTALSIS is the involuntary, wavelike muscle contractions which pass along a tubular
organ such as the bowel, moving the contents along the tube. ANTIMOTILITY DRUGS depress or inhibit peristaltic movement of the bowel, resulting in
delayed passage, or retention, of the contents, including waste materials, organisms and
toxins. Note: for an explanation of controlled, random and blind trials, see="dd42.htm#page4">DD42, p. 4.
|
I. Portnoy, B L, et al., 1976. Anti-diarrhoeal agents in the
treatment of acute diarrhoea in children, JAMA 236: 844.
2. Harris, M J, and Beveridge, J, 1965. Diphenoxylate in the treatment of acute
gastroenteritis in children. Med. J. Austr. 2: 921.
3. Bitar, J, et al., 1970. Diphenoxylate hydrochloride therapy in diarrhoea of
malnourished infants. Arch. Dis. Child. 45: 190.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  5 Page 6 7 5 Page 6 7
Worms and community health
Why bother treating for worms if we want to control diarrhoea?
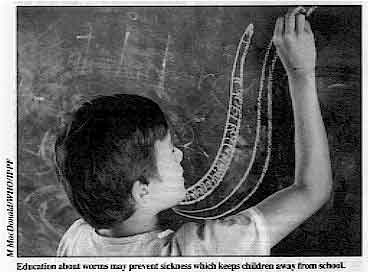 |
Education about worms may prevent sickness which keeps children
away from school. 
roundworm
hookworm
whipworm
|
If you ask a group of health workers to list the causes of diarrhoea, the chances are
that worm infection will not even be mentioned. Yet one of the commonest worms, the
whipworm Trichuris trichiura, has been known for decades to cause chronic
dysentery. Clearly there is a problem in how we perceive the impact of worm infection on
community health. Worms and diarrhoea
A major part of the problem is the tendency to think of infection with the various
helminth species as the single disease entity 'worms'. It would be considered very poor
practice to speak of 'viruses' or 'bacteria' in the same way. Each of the three common
species of intestinal worm (roundworms, whipworms and hookworms) is estimated to infect
more than 500 million people. All have an important impact on public health, but it is
only the whipworm that typically causes diarrhoea, and only the more intense whipworm
infections that result in dysentery. The more worms that are present, the more likely it
is that disease will result. Thus, only a minority of 'worm' infections are associated
with diarrhoea. But because worm infections are so common, this minority of cases will
number in the tens of millions. A second part of the problem is that we have tended to focus on diarrhoea as an acute
problem of children under five years of age. The dysentery due to trichuriasis, on the
other hand, is chronic, often lasting for years. It occurs most commonly among children of
school age. Trichuris dysentery
Acute diarrhoea in children can be fatal and should be tackled first. But success in
helping children to survive to five years of age should not allow us to ignore their
quality of life thereafter. One of the consequences of chronic dysentery is that it causes
children to grow more slowly physically and to become stunted. Studies in schools have
shown that the children with the most intense infections tend to be relegated to the lower
streams; they are considered by their teachers to be less able academically. The worst
affected children may be so disabled by dysentery over a period of years that they hardly
go to school at all. Thus Trichuris dysentery may result in physically stunted children
who are unable to benefit from their schooling. The good news is that something practical can be done. Health education and sanitation
programmes can make an important contribution, just as they can in the control of acute
diarrhoea. More importantly, perhaps, treatment for trichuriasis is very effective in
immediately stopping dysentery and in reversing stunting. Stunted children given an
effective anti-helminthic medicine show spectacular catch-up growth, without the need for
an improvement in diet. So, simple anti-helminthic treatment has similar consequences to
ORT in that it has immediate therapeutic value. If designed as part of a sustained
community programme, anti-helminthic treatment can have the important additional benefit
of preventing further disease. This occurs because the treatment reduces the contamination
of the environment with infective stages, by removing the worms, and so reduces the rate
of reinfection. Children still become reinfected, but it takes a long time for the worm
burdens to build up to the intensity that causes disease. Meeting community needs
Programmes to treat worm infections have other benefits. If, instead of asking health
workers about diarrhoea, you were to ask mothers about health problems in their children,
they would certainly mention worms. They have probably seen their children pass the large
roundworm Ascaris lumbricoides. This worm does not typically cause diarrhoea, but
treatment for trichuriasis requires the use of a broad spectrum anti-helminthic - the
benzimidazoles, albendazole or mebendazole which will expel all the major intestinal
nematodes including the roundworm. A worm control programme therefore deals with a problem
that the community recognises, with obvious benefits in terms of acceptance and
sustainability, not only for the worm control programme but also for community health
programmes in general. Why treat for worms? Because it reduces the health impact of worm
infection, including Trichuris dysentery, and increases confidence in other community
health programmes. It may also improve the quality of life of the children which acute
diarrhoea control programmes have saved. Dr D A P Bundy, Wellcome Trust Research Centre for Parasitic Infections, Department
of Biology, Imperial College, Prince Consort Road, London SW7 2BB, UK; and Dr E S Cooper,
Tropical Metabolism Research Unit, Faculty of Medicine, University of the West Indies,
Kingston, Jamaica.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  6 Page 7 8 6 Page 7 8
Low cost sanitation Lesotho is committed to introducing latrines in every household. Isabel
Blackett describes how this is being achieved. Lesotho's low cost sanitation programme has two separate but complementary parts. The
Urban Sanitation Improvement Team (USIT) in the Ministry of the Interior covers all urban
areas. The National Rural Sanitation Programme (NRSP) in the Ministry of Health does the
same in the rural areas. Both have the same guiding principles, co-ordinate major
decisions and promote the same latrine designs. The national programme is based on several years of pilot work and research. During the
pilot phase, local conditions were evaluated, available and affordable materials were
assessed and socio-economic surveys were carried out. Demonstration models of latrines
were tried and public response to them was monitored. Suitable materials for health and
hygiene education were gradually developed and the use of radio was also explored. The key elements of the programme are:
- an affordable and acceptable Ventilated Improved Pit (VIP) latrine of national design;
- a comprehensive programme of latrine promotion and health and hygiene education;
- latrine construction carried out by the private sector - the government provides
training, follow up supervision and assistance to the builders - no grants or subsidies
are given to householders for sanitation;
- low programme administration costs;
- strong co-ordination between NRSP, USIT and other departments involved in promoting low
cost sanitation.
Provision or promotion? There are several possible approaches to introducing low cost sanitation. One is to
provide all householders with latrines free of charge. However, this requires enormous
resources, and some studies have shown that people provided with free latrines may not use
or maintain them. Another possibility is to encourage people to build latrines by offering
subsidies. This also requires resources, and subsidies have to be targeted carefully and a
way found to determine who should get them.
|
Families are working together in Lesotho to build their own
pit latrines.
The approach taken in Lesotho is to promote and market latrines in such a way that
people want the 'product' (the latrine), and are prepared to pay for it themselves. The
latrine must therefore be highly desirable and affordable, otherwise no matter how good
the promotion, this approach will not work.
|
 |
Affordable Ventilated Improved Pit (VIP) latrines have been designed using a wide range
of materials, so that people can choose a suitable material according to the resources
they have available. In urban areas, a credit scheme is available to enable people to take
a 60 per cent loan and pay it back over two years. Getting the message across
USIT and NRSP have used a variety of methods to promote the construction and use of VIP
latrines. Some have proved to be more effective than others. One of the most effective is radio. This reaches a very wide audience, including those
who cannot read. Drama, quizzes, information programmes, interviews, jingles and
advertisements are all used. Many people have access to a radio and the national station
is popular. Another effective method of promotion uses audio-visual materials - locally made
tape-slide programmes run by a small generator. The programmes are aimed at different
groups including school managers, primary and secondary school pupils, local officials,
health workers, builders and carpenters. They are always used as part of a talk and
question and answer session. Traditionally, people come together in public meetings called
'pitsos'. This is the way
community issues are discussed and solved. At these meetings, the chief or a visitor can
address the group, and questions can be asked. USIT and NRSP community staff often attend
pitsos to talk to people about health issues and reasons for improving their sanitation.
This method is, not surprisingly, more successful in rural areas and small towns than in
the capital city. Printed matter is used as a back-up to radio, audio-visual material and
community work as well as on its own. A promotional T-shirt, sold at cost price, with the
message 'A VIP is good for you' is very popular. Posters, pamphlets and leaflets have also
been produced and distributed. Loan scheme To increase the number of people able to afford to build latrines, a sanitation loan
scheme has been set up. The idea is based on the common practice of making monthly
repayments for furniture, clothes or household items. The full loan amount is paid back
with interest to the Lesotho Bank on a monthly basis over any period up to two years. The client proves her or his commitment to the scheme by a 'deposit' of collecting the
blocks (for the sub-structure) and the sand, and by digging the pit. USIT assesses the
loan application, mainly to ensure that the client can make the repayments. There is no
means-testing and anyone can apply for the loan. In some towns up to 30 per cent of the
latrines have been built using the scheme and repayment records are good. Isabel Blackett, 34 Station Street, Loughborough, Leicestershire LE11 0ED, UK.
|
|
DDOnline Dialogue
on Diarrhoea Online Issue no. 43 December
1990  7 Page 8 7 Page 8
Questions about SSS
I am a member of a team of ORT instructors, and recently found myself unable to answer
a simple question from a trainee about sugar-salt solutions (SSS). Our national ORT policy
gives the recipe for SSS as ten level teaspoons of sugar and one level teaspoon of salt
for one litre of drinking water. But the WHO guidelines we have are eight level teaspoons
of sugar and one level teaspoon of salt for a litre of drinking water. Which one is right? Secondly, some children can hardly tolerate any oral feed, especially if they are
anorexic. We find it difficult to maintain those patients who are likely to develop
hypokalaemia (potassium deficiency) as SSS is the only solution readily available. I have
started adding mashed bananas or fruit juice to the SSS in the hope of increasing
potassium intake. Please would you give more information about this? Abdul-Rahman Umar Pella, Primary Health Care HQ, PMB 5, Song, Gongola State,
Nigeria.
Dr Nate Pierce of WHO replies: Experience has revealed important problems that limit the usefulness of sugar-salt
solution (SSS) as a home fluid for diarrhoea. One is that there is no single agreed recipe
for making SSS. A second is that mothers often prepare SSS incorrectly, owing either to
mistakes in measuring the ingredients, or because they do not remember the recipe
correctly. The danger is that SSS will be prepared with too much sugar or salt, or too
little water. This creates 'hypertonic' solutions that can cause diarrhoea and dehydration
to become worse, because the fluid 'draws' water out from the body into the bowel. WHO
gives preference to home fluids that contain cooked cereals, such as rice water or cereal
gruel, rather than sugar, because these are not likely to be hypertonic. As the starch in
these fluids is digested, glucose is released and rapidly absorbed, together with water
and salt. If SSS is used, WHO advises that it contain 3 grams of salt (about one level
teaspoon) and 18 grams of sugar (4 to 5 level teaspoons) per litre. By recommending
this lower amount of sugar, it is less likely that measuring mistakes will cause fluids to
be dangerous. WHO does not advise adding foods to SSS or ORS solution, as this could confuse mothers.
It is quite acceptable, however, to alternate the giving of fluids and food, for example,
some sips of fluid followed by some mashed banana, and then more fluid or juice. In
addition to providing energy and protein, foods are an important source of potassium,
which is lost during diarrhoea and is not present in SSS. Besides bananas and fresh
fruits, good sources of potassium are cooked pulses, green coconut water, and dark green
leafy vegetables. Training pharmacists
During the past year, I have been working with village pharmacists to provide follow up
training for them and to help them improve their understanding of appropriate drug use.
Apart from malaria, diarrhoea is the most common problem which villagers bring to the
pharmacists here. Most mothers and pharmacists feel that diarrhoea is not dangerous,
because it is so common and because most children recover in a few days. For mothers here,
who carry their babies on their backs, a child with diarrhoea is a nuisance. What mothers
want is for the diarrhoea to stop. This is one reason why anti-diarrhoeal drugs are used
so widely, and why ORS is less popular. I have found that it is better to concentrate on teaching pharmacy workers more about
the signs and dangers of dehydration, so that they understand why and when ORT is really
important. I have also tried to teach that the antimotility drugs which are widely used
here should never be given to children less than eight years old. The best explanation I
can give seems to be that these drugs only treat the diarrhoea and not the cause. This
helps with the pharmacists, although not usually with the mothers. I have also started to
encourage health workers to teach mothers to give boiled rice water as a rehydration
drink. If rice based solutions can reduce the duration of the diarrhoea, this will make
ORT more attractive to mothers. One other problem, which is extremely common here, arises when a course of drugs
lasting for five days needs to be prescribed, for example when antibiotics are given to
treat bloody diarrhoea. The person who has to pay for the medicine usually the parent of a
sick child - will haggle with the pharmacist to bring down the cost of the treatment. This
often means that the parent persuades the pharmacist to sell them enough drugs for only
two or three days instead of enough for five. With too few tablets, the child's symptoms
may be suppressed for a short time, but then the disease returns. It is extremely
important for pharmacy workers to understand that a course of medicine should not be cut,
but this will always be difficult while people cannot easily afford the price of the
drugs. Kenneth Gilbert MD, Institut des Affaires Culturelles, 01 BP 3970, Abidjan 01, Cote
d'Ivoire.
Correction On="dd41.htm#page8">page 8 of issue 41 of Dialogue on Diarrhoea, the
reply from Dr Nate Pierce of WHO to the letter entitled 'Does ORS treat diarrhoea? '
should have read as follows: "Drs Meng and van Bruggen are correct that ORS does not
cause diarrhoea to stop, but neither do 'anti-diarrhoeal drugs'. It is better to tell the
parent: This medicine (ORS) will help to make your child feel better and be stronger. It
will not make the diarrhoea stop; no medicine can do that. But do not worry. The diarrhoea
will stop by itself in a few days. In the meantime, giving ORS and continuing to feed your
child is the best way to keep him healthy."
|
| PHC courses in the UK A revised edition of the AHRTAG directory
listing all UK short courses (less than six months) in primary health care is available
for 1990 to 1991. Details of 68 courses are listed, along with suggested funding sources
and useful publications. Cost UK £3.50 plus postage (£0.35 to UK;£0.85 to Europe;
£1.75 outside Europe). Contact: Margaret Elson, AHRTAG.
|
Scientific editors Dr Katherine Elliott and Dr William Cutting
Managing editor Kathy Attawell
Assistant editor Nina Behrman Editorial advisory group
Professor J Assi Adou (Ivory Coast)
Professor A G Billoo (Pakistan)
Professor David Candy (UK)
Professor Richard Feachem (UK)
Dr Shanti Ghosh (India)
Dr Michael Gracey (Australia)
Dr Norbert Hirschhorn (USA)
Dr Claudio Lanata (Peru)
Professor Leonardo Mata (Costa Rica)
Dr Jon Rohde (USA)
Dr Mike Rowland (UK)
Ms E O Sullesta (Philippines)
Professor Andrew Tomkins (UK)
Dr Paul Vesin (France) With support from AID (USA), ODA (UK), UNICEF, WHO Publishing partners
BRAC (Bangladesh)
CMAI (India)
CMU (China)
Grupo CID (USA)
HLMC (Nepal)
lmajics (Pakistan)
ORANA (Senegal)
RUHSA (India)
Consultants at University Eduardo Mondlane (Mozambique)
|
Issue no. 43 December 1990
Page Navigation
This edition of Dialogue on Diarrhoea Online is produced by Rehydration Project. Dialogue on Diarrhoea was published four times a year in English, Chinese, French, Portuguese, Spanish, Tamil,
English/Urdu and Vietnamese and reached more than a quarter of a million readers worldwide. The English edition of Dialogue on Diarrhoea was produced and distributed by Healthlink Worldwide. Healthlink Worldwide is committed to strengthening primary health care and
community-based rehabilitation in the South by maximising the use and impact
of information, providing training and resources, and actively supporting
the capacity building of partner organisations. - ISSN 0950-0235 Reproducing articles
Healthlink Worldwide encourages the reproduction of
articles in this newsletter for non-profit making and educational uses. Please
clearly credit Healthlink Worldwide as the source and, if possible, send us a copy of any uses made of the material.
|
updated: 23 August, 2019
|